3Derm: A Dermatology Triage System

Using digital technology to improve access to healthcare for those who need it the most.
Insufficient Access to Healthcare
Skin cancer is the most common cancer: about 3.3 million Americans are diagnosed with skin cancer each year2 and 1 in 5 Americans develop skin cancer during their lifetime.1 But skin cancer can be detected early and fatal prognoses can be avoided if patients regularly examine their skin and report any changes to their doctor in a timely manner.
Unfortunately, even when patients discover a concerning rash or mole, they are not guaranteed access to care, prompt or otherwise.
On average, patients wait 29 days for a dermatology visit; those on Medicaid or in certain geographies often wait 100+ days.1,4 “Reducing the wait time for skin cancer diagnosis by even a week can result in a significant decrease in mortality.”4
And, access to health insurance “does not always guarantee access to a physician,” especially for some of the most vulnerable population.3 A 2014 survey of 15 metropolitan US markets (administered by Merritt Hawkins) reveals the following:3
- Medicaid is not widely accepted: 45.7% average acceptance rate, with significant variation across markets
- Medicare is more generally accepted, but does not ensure access:0% average acceptance rate, more standardized across markets
Today’s “Store and Forward” Telemedicine Market
Advances in Internet connectivity have allowed for the rise of telemedicine – the exchange of medical information via electronic communication. Now doctors can receive digital images of patient data sent from remote locations and use those images to “render[] medical opinion or diagnosis” without ever having to see the patient in person.5
Consequently, telemedicine has the potential to be a transformative tool, broadening healthcare access to traditionally underserved populations. It presents an exciting opportunity to provide better care for those who live in rural areas and those with limited income and resources.
3Derm Overview
Founded in 2012
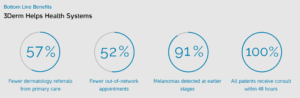
Mission: Create a practical dermatology triage system “designed to expedite appointments for the most urgent consults while screening out benign concerns”4
“Without a reliable dermatology triage system, thousands of patients requiring urgent intervention wait alongside millions with benign conditions.” – 3Derm1
Concept: 3D skin imaging system that “captures and delivers the same 3 views a dermatologist uses in an exam room, making remote visits virtually indistinguishable from current practice.” 1 This allows for primary care physicians to quickly (and remotely) scan hundreds of images and prioritize dermatology referrals based on need.
Strategy: Enter dermatology care supply chain as intermediary that provides value to each member of the chain.
Early Success: Clinical study showing efficacy and accuracy of 3Derm technology in n=350 patients. “Dermatologists reading 3Derm images identified malignant and benign legions on par with dermatologists diagnosing in-person.”1
The Physician, Provider & Patient Promise
3Derm provides value across the entire supply chain by improving quality and efficiency while reducing cost,7 and helps efficiently allocate scarce resources to meet the most urgent demand.
Physicians
- Improved clinical outcomes
- Improved patient satisfaction
- Better leveraged time / more efficient referrals (reduced number of in-person visits for patients with benign conditions and better ability to prioritize care for those in urgent need)
- More flexible hours
- Higher practice revenue
Insurance Provider
- Prevent disease progression, which can be exceptionally costly
Patients
- Greater access to care when needed
- Improved convenience (can avoid going to the doctor when not urgent)
Next Steps 3Derm Should Consider Implementing
3Derm will need to continue to develop its network of clinics and hospital systems and strengthen relationships with dermatologists to ensure that they will make room for for high priority patients… even those without private coverage.
Additionally, there are two main strategies 3Derm can pursue to improve product adoption
- Use data to convince insurance providers to improve reimbursement: As mentioned above, telemedicine is not consistently covered for all patients, least of all those on Medicaid. Consequently, 3Derm should invest in health economics and outcomes research (HEOR) studies to show insurance providers the potential for substantial cost-savings and improved health outcomes presented by this technology. Additionally, 3Derm can partner with other telemedicine companies to lobby for expansion of Medicare and Medicaid coverage of telemedicine.6
- Reduce barriers to interstate use of telemedicine services: Current licensing laws impede interstate use of medical services (40 states require all physicians to have a full in-state medical license in order to practice teledermatopathology). Consequently, 3Derm should partner with other telemedicine companies to reduce additional licensing requirements and, in the meantime, ensure their network contains specialist providers in all states across the country.5
(754 Words)
- Company Website. Retrieved from: https://www.3derm.com/
- Skin Cancer Factsheet. Retrieved from: http://www.cancer.org/cancer/cancercauses/sunanduvexposure/skin-cancer-facts
- Merritt Hawkins 2014 Survey: Physician Appointment Wait Times and Medicaid and Medicare Acceptance Rates. Retrieved from: http://www.merritthawkins.com/uploadedFiles/MerrittHawkings/Surveys/mha2014waitsurvPDF.pdf
- 3Derm Teledermatology System Makes Commercial Debut at ATA 2016 Conference. Retrieved from: http://www.marketwired.com/press-release/3derm-teledermatology-system-makes-commercial-debut-at-ata-2016-conference-2124365.htm
- Giambrone, D. et al. (Oct 2014). Obstacles hindering the mainstream practice of teledermatopathology. Retrieved from: http://www.sciencedirect.com/science/article/pii/S0190962214014005
- Beck, M. (June 2016). How Telemedicine Is Transforming Health Care. Retrieved from: http://www.wsj.com/articles/how-telemedicine-is-transforming-health-care-1466993402
- Collier, G. (Jul 2016). Economic Driver: 3Derm skin cancer imaging is chosen for state pilot program. Retrieved from: http://www.telegram.com/news/20160710/economic-driver-3derm-skin-cancer-imaging-is-chosen-for-state-pilot-program



I agree completely that dermatology is a field where asynchronous telehealth visits (i.e. the patient takes photograph of rash and provides brief history to MD via live discussion or via recording) is an excellent way to solve the issue of triage in a group of say 1,000 patients waiting to see the dermatologist, 995 of whom have very benign lesions and 5 of whom have more concerning malignant lesions. The problem I see here is that it doesn’t solve the fundamental problem – lack of dermatologist supply on a national level. Yes, it may solve local distribution problems (i.e. not enough dermatologists in Nebraska, too many in New York City) but not the national problem. I would argue that the primary need here is for automated detection algorithms (i.e. a la Watson) so be able to “interpret” images of moles and possible melanomas with a high degree of sensitivity (i.e. no false negatives) and specificity (i.e. no false positive). A friend has been working on this (http://jamanetwork.com/journals/jamadermatology/fullarticle/1741083) but there is unfortunately a tremendous variety in quality between apps that do this work and they are in fact going to end up being FDA regulated given the risks here.
Taki
Telemedicine is definitely a field that technology could create value to consumers in healthcare. In terms of adoption of this service, one critical component would be to alter consumer behavior so that consumers will make immediate dermatology visit to their PCP, which I assume is not common behavior at the moment.
I think this is a great advancement toward detecting cancer early. That being said, I wonder if more can be done to prompt individuals to seek medical attention in the first place. Those interested in using telemedicine are presumably already quite responsible and aware of certain health risks – but I continue to see a strong barrier for individuals who are not as well informed or motivated to seek medical attention.
Anonymous, I really enjoyed reading about how 3Derm has the capability of better matching supply of dermatologists and demand for their services. I am equally optimistic about how telemedicine is playing a similar role in behavioral health. Behavioral health care shares some of the traits you described in dermatology (including, long wait times and inconsistent reimbursement) but also has the barrier of stigma that unfortunately dissuades some patients from seeking treatment. Telemedicine has the advantage of making behavioral health services more discrete, which may encourage more individuals in need to seek them out. As with dermatology, there are regulatory barriers that need to be overcome; but I am encouraged that telemedicine will eventually be a solution to improving quality and acess to behavioral health care while reducing costs.
(http://www.forbes.com/sites/brucejapsen/2016/06/30/telemedicine-companies-see-mental-health-as-next-frontier/#449d087395ac)
I love the use of asynchronous telehealth in targeted cases! It exemplifies efficiencies in a cost-laden and time-intensive system that we can address through digital innovation. In the case of 3Derm, though, it still leaves something to be desired. 3Derm currently connects primary care providers to specialists and thereby conserves dermatologist hours but as you note, a lot of the barrier is in getting the patient to even see a doctor in the first place. As 3Derm itself notes (1), the company tried to develop a mobile device-compatible imaging program a few years ago that resulted in catching 75% of malignancies but missed 25%. As mobile hardware innovation has occurred at a significant pace (as one example: iPhone cameras today are at a multi-fold resolution enhancement relative to five years ago), I would support 3Derm in continuously investing in mobile R&D to cut out even the PCP visit from the diagnosis process, connecting the patient in his home with a dermatologist on the other end.
References:
1. http://www.telegram.com/news/20160710/economic-driver-3derm-skin-cancer-imaging-is-chosen-for-state-pilot-program
Looks like I’m late to the commenting game on this one. Coming from a family of dermatologists, (both my mother and sister are practicing dermatologists), I have seen firsthand some of the 50+ day wait times to get into a dermatologist, when most of the appointments blocking a person from seeking care are routine consults and skin checks. While I agree with NJG on the importance of urging patients to seek care in the first place, I don’t actually see this as a major risk for the majority of skin cancer patients, most of whom have struggled with skin issues preceding the cancer. My concern with 3Derm’s business model is it’s likelihood to succeed in the increasingly competitive telemedicine space, particularly when it is currently a sole use product for dermatology applications. I would think that private practitioners may be attracted to the product since it is customized to their needs, but I’d be concerns about whether larger providers such as hospitals would be likely to enroll given their need for products that work across a range of specialties.
I also wrote about how the healthcare industry is becoming more digitized and I definitely agree with the sentiment that barriers between states and between competing digital providers need to be overcome to get the true benefits of these new networks. The more information that can be shared digitally (in a safe and privacy protected way) the more the patients and hospitals/doctors will realize the benefits of these new services.
One questions I had about 3Derm’s services is if dermatologists offices need to invest in any additional equipment in order to receive and analyze the preliminary results? It seems clear that the PCP’s need to invest in this equipment so I am curious how these costs are allocated between the different parties that are involved.
While the 3Derm system offers differentiated value today, one chief concern I have with their business model is the reliance on their physical system for that differentiation (see product overview on https://www.3derm.com/). Many telemedicine competitors are emerging in the space, and several use iPhone / smartphone cameras in order to relay information to dermatologists. While the 3Derm argument is currently that those photos are not high enough quality, the current rate of technological advancement is not on the company’s side. At some point in the near future, 3Derm’s physical camera system is going to be obsolete or at least no longer a competitive advantage. At that point, their offering will really hinge on whether they have a sufficient network of PCPs and dermatologists to remain sticky in the marketplace. This may be challenging. As BAL points out, 3Derm is currently competing with a growing number of telemedicine solutions, many of which are compatible with services beyond just dermatological triage. Telemedicine triage is likely to play a role in the future and as the author pointed out, holds great promise for increasing access for low income patients (among others). I am just not sure if 3Derm can gain market share fast enough to be a major player in that market. Perhaps an acquisition by a larger telemedicine player (like https://www.teladoc.com/) is in their near future or their best way forward.
The trouble with 3Derm and telemedicine more generally seems to be the trust that the patients currently have in a system that doesn’t involve the physical presence of a medical professional(1). This could be addressed with patient education, but will likely take additional training costs and time.
(1) http://hitconsultant.net/2015/07/15/telemedicine-patients-wouldnt-trust-a-diagnosis/
The trouble with 3Derm and telemedicine more generally seems to be the lack of trust that the patients currently have in a system that doesn’t involve the physical presence of a medical professional(1). This could be addressed with patient education, but will likely take additional training costs and time.
(1) http://hitconsultant.net/2015/07/15/telemedicine-patients-wouldnt-trust-a-diagnosis/