Concentrating prostate care in the Netherlands
If the Netherlands had their prostate care organized like the Martini Klinik in Germany it could prevent 400 cases of incontinence, 1000 of impotence and more than 60 complications a year.
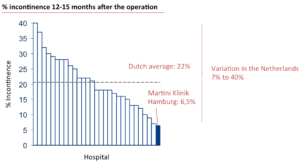
The differences in the quality of care between hospitals performing a radical prostatectomy in the Netherlands are enormous. For example the probability of becoming incontinent ranges from a 7% (best case) to 40% (worst case). With an average probability of 22% this is far higher than for example Germanys best practice: The Martini Klinik (see HBS business case by Michael Porter) in Hamburg, at only an hour flying time from Amsterdam, with only a 6.5% probability. For impotence the numbers are quite shocking as well, with an average Dutch probability of 74% compared with a 34.7% outcome at the Martini Klinik. Severe complications count for 2.7% patients in the Netherlands and 0.14% in the Martini Klinik.
Prostate cancer occurs in the life of 1 out of 10 men in the Netherlands. It is the most common form of cancer under men. Due to an aging society the total number of men needing a radical prostatectomy is expected to rise in the near future. The chance of survival is quite high, though the quality of life after the operation is a significant aspect considering the chance on becoming incontinent or impotent. The possibility of becoming impotent or incontinent drops drastically with the experience of the urologist preforming the procedure.
The Martini Klinik performs 2,225 procedures a year. The minimum number of operations by an individual urologist a year is 250. 2,582 radical prostatectomies were performed in the Netherlands in 2015 by 37 hospitals. The lowest number of operations performed by a hospital is 5 the highest 272. It is not likely that any of the urologists performing this procedure in the Netherlands will reach the minimum standard of 250 operations a year. It seems that poor quality is the outcome of far too low volumes and with that, lack of experience by the urologists. Urologists are well aware of these facts but due to competition between hospitals and healthcare insurers nothing is happening.
As the largest healthcare insurer we find it time to improve outcome for our insured and concentrate prostate care in two hospitals in the Netherlands in 2019. With two centers with each 6 urologists there is sufficient bundling of expertise and the number of 200 – 250 procedures by each urologist can be reached. Holding 31.5% of the Dutch market, it is for us of no use doing this alone. So we filed a request at the Dutch Federal Trade Commission to be allowed to work together with three other healthcare insurers, together holding 88.47% of the market, to concentrate prostate care in two hospitals.
There is no way of knowing what the Federal Trade Commission will decide. Suppose we don’t get a green light on working together or concentrating prostate care in two hospitals. What should our way forward be? Given the current outcomes, doing nothing is no option.




Are you suggesting that the urologists at other centres/ hospitals are not competent- and all the patients must for prostatectomy must come to the 2 hospitals. I would argue that the patients should have access at the point of need and the care must not be concentrated away from them.
By narrowing down the access – you will be increasing the wait lists and also increase pressure on other resources in those hospitals.
I would say that instead of concentrating prostate care in two hospitals you should be looking at maximising access for your patients at their point por need and take the care to them.
This is the day and age of Tele medicine and robotics- think outside the box.
Thank you for your comments. Concentrating prostate care in only two hospitals is exactly what we are proposing. The only way to make sure that urologists have enough experience is if they conduct this procedure 200 – 250 times a year. Even if they use the Da Vinci the only way to deliver quality is in experience which means quantity. With about 2500 cases a year and an group of expertise needed of around 6 urologists that leaves room for 2 centers. Your right, waiting lists might become an issue in dedicating urologists only to these procedures. It makes the pool of experienced specialists smaller. Considering taking care to peoples home you are making an excellent point. The total patient journey with diagnostics and follow-up takes about 10 years. Only the actual operation, which takes two days, we want to concentrate at two hospitals. In a survey by the Dutch Prostate Association 91% of the responders were willing to travel further to a hospital with more experienced specialists.
A ground breaking approach! is concentration really the only key success factor or do cultural differences also play a role and would the Netherlands need a different approach?
This is a very interesting and timely issue. Minimum volume “pledges” have become a topic of substantial discussion in many surgical specialties. See for example this article from NEJM on one such effort: http://www.nejm.org/doi/full/10.1056/NEJMp1508472?af=R&rss=currentIssue
One question is whether the 250 procedures/surgeon threshold you mention is simply appying the Martini Klinik standard or has it been shown to be the optimal minimum volume in other studies. It strikes me as a bit higher than recommended minimum volumes in other procedures, but this may represent a particular characteristic of prostate procedures.
Thank you for the article. I do agree that minimum volumes are not always the panacea for quality in outcomes. In this particular case we are talking about elective care in a region half the size of the state of New York with 17 million habitants. I don’t think the dilemma of improving the quality of low volume hospitals is a consideration. With all prostate care concentrated in two centers the maximum traveling time will be about an hour and a half. There is no need to leave any volume behind in other hospitals.
There is a lot of discussion (read confusion) about the minimum volume needed for this procedure. The Dutch Urologist Society (which is not a scientific body) uses 20 procedures a year per hospital location as the minimum volume. The minimum volume set by the European School of Oncology is 50 operations per hospital location. http://www.eso.net/images/ejc.pdf These norms say nothing about the number of procedures preformed by an individual specialist.
Intuitive surgical, the producer of the Da Vinci robot, sets a minimum standard of 250 operations per urologist a year being able to use this equipment independently. And for a significantly less complex procedure like a colonoscopy the European Guidelines for Quality Assurance use 300 procedures per specialist as minimum norm. http://www.kolorektum.cz/res/file/guidelines/CRC-screening-guidelines-EC-2011-02-03.pdf
Actually we are looking for the optimum and not the minimum volume. Using a volume between 200 and 250 procedures a year in line with the Martini Klinik as a best practice and in analogy with the guidelines for colonoscopy and the use of the Da Vinci robot.
An interesting article in the NEJM about the relation between volume and outcome on prostate cancer http://www.nejm.org/doi/pdf/10.1056/NEJMsa011788
Interesting topic and certainly a challenge. Similar to the question of whether patients should be in specialty ICUs or general ICUs, there is clearly a volume phenomenon that improves outcomes for a wide variety of reasons that extend beyond just the physician. I think that centralizing the care to a few centers is appropriate, especially in a geographic region that would not place huge travel burdens on patients. The volume challenge is getting worse as surgeons and other procedure based specialists are coming out of training with much less experience than the earlier generations. Whenever I have been asked to perform a spinal tap on a child where others have failed, I have to remind myself that the younger generation trained in an era where vaccination rates are high. As a resident in a really busy pediatric ED in the 1980s I could do as many as 10 spinal taps in one shift. Now some trainees finish a three year residency not having done ten in their whole time. The martini clinic is a great example of organizing the care around the patient with everything truly designed to improve the quality of care, not the ease of the providers and the improvements in outcomes. The variation in surgical programs can be quite huge and really shouldn’t be. A lot can learned from the Martini clinic approach even if you don’t limit to two or three centers in terms of how they structure care, how they review performance (most american hospitals are no where near as rigorous at evaluating performance and taking steps to ensure people improve to the benchmark or get help).
Thank you for your reaction Steve. I find your personal perspective on the connection between prevalence, experience and travel distance very interesting. It seems that healthcare adapts slowly to some new circumstances.
I totally agree on your remarks made about the Martini Klinik. Besides concentrating volumes, there is a lot to be learned from them. I was very lucky to be able to visit them last year and meet with most of their medical staff. I was really impressed. It is a culture of learning and improving. I will never forget what one of the founders of the clinic said: ‘this culture started with breaking down the specialist’s ego’. Only after that there could be a culture of transparency and learning.
The way they keep track on outcome, discuss these outcomes directly with as a result a much steeper learning curve for new specialists joining the team, is an example for healthcare providers on both sides of the ocean. It also raised the question to me: why is this not the standard for the rest of Germany?
Great conversation so far.
I would agree that concentrating patients in fewer hospitals would allow for better care, related to greater expertise gathered through greater patient volumen.
The issue in my opinion is how to best achieve this concentration:
1. Allowing patient´s freedom of choice.
2. Disclosing medical results among, not only the medical community, but also among the patient population –> full medical transparency so that patients will choose the fewer hospitals with best results.
3. Creating bundled payments for prostate cáncer intervention, including in these bundled payments complication rates and clinical outcomes of the best practicing hospitals (severe compolication rates 0,14%, incontinent rate 35%, for example) –> this would place a greater financial burden on those hospitals that do not adhere to these rates, making them pay for the complications.
** Financial burden and patient´s freedom of choice would place a greater strain on those underperforming hospitals, causing a more natural patient flow selection towards best achieving medical centers.
Thanks for your suggestions. I do agree with number 2 and 3. Especially paying for the bundle might be in place to add more value in the chain of prostate care. Number one, patient’s freedom of choice is something I am experiencing a growing difficulty with. I think it should go hand in hand with number 2, full medical transparency. But even with full medical transparency if freedom of choice leads to significant worse outcome it is time to act (like in the London Stroke Care case). My personal opinion is that freedom of choice is the lesser one if the patients quality of care/life is at stake, as is the case in this example.
Hi Erik,
Being from the Netherlands I encourage you to keep fighting for concentration. What foreigners might not know is that the Netherlands is such a smal country that you are max 1.5 hrs by car away from one of the two anticipated centers.
I guess you have to be bold and pursue. If two is not allowed go for three. Ask the urologists/medical centers to come up with proposals and select the top 2 (or 3).
Thanks. I think you are right, although it will be very disappointing to start out with three centers, knowing that Martini is handling almost the same volume as the whole of The Netherlands.
Hi Erik,
This is not a management issue, but a national health care policy issue. That means that you have to deal with all kinds of different interests from different parties within the helath care system. At the least, the interests of parties involved will not all be ‘entirely alligned’. For sure, the patients’ health is paramount to everybody working in health care, but when the consequences of a new medical treatment insight is obviously not in the interest of hospitals in general or to a specific group of medical professionals as a whole, defense strategies can be anticipated.
Your case is quite stunning with regard to these seemingly clear medical facts. I wonder therefore in the first place how controversial these facts are ? How broad are they accepted ? What is the opinion / reaction of the national society of urologists on this issue ? They risk to position themselves as merely stakeholders of the urologists, if a non supportive reaction is not substanciated with thorough arguements.
The case reminds me of the imminent concentration of childrens oncology in the Netherlands. I think that the some high esteemed paediatricians together with some national patient organisations, started a discussion, where no other paediatrician in the end could keep himself apart from.
In the case of a patientgroup mainly consisting of man around their sixties, it cannot be too hard to have a well-organised and well-informed lobby organisation, actively influencing the public opinion on this issue.
So, as an insurer, I would avoid direct lobbying, but would strongly facilitate the debate between professionals/urologists in public settings. And let the patient organisations participate, aside scientific journalists; ‘Let the spirit out of the bottle’.