When Epic Digitization is Not So Epic

Epic was on the digitization forefront when it was founded in 1979 and has become a billion dollar business as a result. But now that electronic medical records are the norm, can Epic continue to rely on its large market share or is it time for the giant to find a new edge?
Building an Epic industry
You might not have heard of Epic Systems, but their software has likely made it possible for you to get the treatment you needed if you’ve ever visited a CVS Minute Clinic, Kaiser Permanente, or large teaching hospital. Epic is the leading electronic medical record (EMR) provider in the U.S.–with 12.4% market share in 2016–in part because it was founded in 1979 before “digitization” was a business phenomena, and more recently because of wide scale health care reform that has invested over $20B in technologies to improve patient outcomes [1, 2]. Epic has continued to grow because of its ability to function in hospital and clinic settings alike, though its critics claim it lacks the dynamism and transparency needed to be a robust tool. This prompts the question; when can we move beyond praising digitization itself and begin to demand more from tech enabled products?
When operating models and the operating room don’t mix
As the first EMR, Epic’s software has become the “‘de facto standard among the more complex academic health centers and multispecialty medical groups,’ says Dr. John D. Halamka, chief information officer of Beth Israel Deaconess Medical Center and a professor at the Harvard Medical School. [3]” While traditional network effects rely on the market to link an increase in one stakeholder group–hospitals and clinics–to drive the increase in another–number of patients in the system–policy also played a huge role in Epic’s network growth. In order to meet the interoperability standards laid out by the Centers of Medicare and Medicaid Services, providers have been incentivized to adopt EMRs that enable secure transfer of patient data across traditional silos like points of care or networks, per the timeline below [4]:
What’s notable about this plan? It worked: from 2008 to 2014 the percentage of hospitals using digital records shot up from 9.4 to 75.5 [5]. To that end, hospitals and clinics alike have often found their hands tied to join Epic’s network in order to share patients with health care giants that can afford the system’s price tag.
Is digitizing enough to “do good?”
Though Epic prides itself on an operating model that focuses on attracting best in class talent and incorporating end-user feedback, those on the other side of the screen frequently share dissenting opinions. Further cementing that Epic’s value proposition is that users should only ever learn to use an Epic EMR, in 2008, 28 of the software giant’s competitors formed the CommonWell Health Alliance Partnership in order to promote interoperability amongst various providers [6]. Epic’s abstention signaled its focus on user acquisition so that information could be traded within the confines of its own records and not beyond; what’s more, Epic charges hospitals and clinics a fee to transfer limited information to non-Epic records and, prior to a 2014 Senate hearing, charged patients $2.35 per year to request access to their own medical record requests [7].
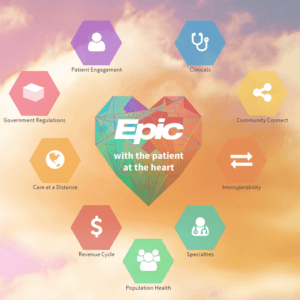
According to employees, Epic’s business model offers its users a comprehensive electronic platform to store, access, analyze, and transfer patient related data. The product, to them, is maximizing health care outcomes and inherently holistic and good in nature–just look at the heart related imagery they use to define their product [8]:
These same employees, however, are quick to share the business’s true operating model: “If you called up any of Epic’s almost 10,000 employees in the middle of the night and asked them the motto, they would recite without hesitation, ‘Do Good. Have Fun. Make Money.’ In that order,” says Peter DeVault, EPIC’s vice president of interoperability [9].
It’s no wonder then that Epic’s customers take issue with a software that is purported to provide value in the form of seamless information storage, analysis, and sharing but instead creates major road blocks that are counterproductive to a system reliant on patients seeing multiple doctors over their lifetime. In 2014, one physician told the New York Times “we’ve spent half a million dollars on an electronic health record system about three years ago, and I’m faxing all day long. I can’t send anything electronically over it,” while in 2015 another touted, “what you hear is that, if you were to buy the best of breed no one would ever choose Epic…but using Epic is easier than trying to piece together better options from various software vendors” [10]. In a world where health record digitization has become the norm, Epic’s value is its begrudging network rather than a sleek product. The firm must focus on its first mission–to do good–and recognize that digitizing records is not the benevolent service it once was. Epic must do more to enable interoperability and ease of use that will truly build a health care system that values patient outcomes through data sharing.
Words: 800
Citations
- Caldwell, P., 2015. We’ve Spent Billions to Fix Our Medical Records, and They’re Still a Mess. Here’s Why.. Mother Jones, [Online]. Available at: http://www.motherjones.com/politics/2015/10/epic-systems-judith-faulkner-hitech-ehr-interoperability [Accessed 14 November 2016].
- SK&A, (2016), EHR Vendor Market Share By Practice Size [ONLINE]. Available at: http://www.skainfo.com/reports/physician-ehr-software-usage [Accessed 14 November 2016].
- Freudenheim, M., 2012. Digitizing Health Records, Before It Was Cool. The New York Times, 14 January 2012. Available at: http://www.nytimes.com/2012/01/15/business/epic-systems-digitizing-health-records-before-it-was-cool.html [Accessed 14 November 2016].
- American Hospitals Association, (2015), CMS Medicare and Medicaid EHR Incentive Programs Milestone Timeline [ONLINE]. Available at: http://www.aha.org/advocacy-issues/hit/mu/overvw-time.shtml [Accessed 14 November 2016].
- Charles, D. , Gabriel, M. , Searcy, T. , 2015. Adoption of Electronic Health Record Systems among U.S. Non Federal Acute Care Hospitals: 2008-2014 . ONC Data Brief, [Online]. 23, 1-10. Available at: https://www.healthit.gov/sites/default/files/data-brief/2014HospitalAdoptionDataBrief.pdf [Accessed 14 November 2016].
- McCann, E., 2015. Epic trades jabs with CommonWell Health Alliance. HealtchareITNews, 14 November 2016. http://www.healthcareitnews.com/news/epic-vs-commonwell-showdown
- U.S. Senate Committee on Health, Education, Labor & Pensions. (2015). America’s Health IT Transformation: Translating the Promise of Electronic Health Records Into Better Care. [Online Video]. 17 March 2015. Available from: http://www.help.senate.gov/hearings/americas-health-it-transformation-translating-the-promise-of-electronic-health-records-into-better-care. [Accessed: 14 November 2016].
- Epic Systems. 2016. Clinics. [ONLINE] Available at: http://www.epic.com/software#Clinicals. [Accessed 14 November 2016].
- Caldwell, P., 2015. We’ve Spent Billions to Fix Our Medical Records, and They’re Still a Mess. Here’s Why.. Mother Jones, [Online]. Available at: http://www.motherjones.com/politics/2015/10/epic-systems-judith-faulkner-hitech-ehr-interoperability [Accessed 14 November 2016].
- Creswell, J., 2014. Doctors Find Barriers to Sharing Digital Medical Records. The New York Times, 30 September 2014. Available from: http://www.nytimes.com/2014/10/01/business/digital-medical-records-become-common-but-sharing-remains-challenging.html. [Accessed: 14 November 2016].



I definitely agree with your assessment about Epic’s interoperability issue. In the past, it seems like Epic was able to rely on its scale and ensuing network effects, besides its technical capabilities, to acquire new customers onto its platform. However, as competitors such as Cerner band together to form the CommonWell Alliance to promote information sharing through interoperable systems, Epic will continually face an uphill battle in maintaining its own separate ecosystem and charging its customers to manually transfer data to other health systems to follow patients’ medical journeys. As I wrote in my post, Epic recently lost a major Department of Defense contract bid in 2015 and analysts attributed not just Epic’s price tag but also its lack of interoperability as key factors for the decision (http://hitconsultant.net/2015/08/03/dod-ehr-contract-will-it-impact-the-larger-ehr-market/). Time will tell, but I’m willing to bet that continued revenue hits such as the loss of the DoD contract will put additional pressure on Epic to become a better team player in the EMR space.
Fascinating article, thank you for writing MRP!
As a user of both Epic and other EMR systems, I think this article is spot on. While clinicians are constantly told that Epic will enable us to better collect and analyze patient information, the user-interface is typically clunky and finding information about previous appointments or hospitalizations (especially if they are out of network) is incredibly tedious if at all possible. We are also told that Epic greatly simplifies the billing and administrative functions of a patient’s visit, something that seems to driving the expansion of Epic more than any of its clinical systems.
While I lack any insight into the strategic decisions behind the adoption of Epic, I do know that BIDMC, the only Harvard teaching hospital not a part of Partners Healthcare, recently chose to go in another direction. Partners spent more than $1 billion to adopt Epic at all of its sites. Rather than foot a similar bill for a lackluster program, BIDMC partnered with Athenahealth to create and implement an alternative EMR. BIDMC has a proprietary EMR (webOMR) that it produced in-house over the years. While webOMR has only a fraction of the functionality of Epic, it was designed with the clinician in mind, and is simple to use. In the deal, Athenahealth will further develop the capabilities of webOMR, which it can then market to other healthcare systems. This system is expected to be significantly cheaper than Epic and will be able to communicate with other IT systems. Hopefully this partnership and others like it will incentivize Epic to improve its produce with all stakeholders in mind–patients, clinicians, insurers, administrators, etc.
While I agree that Epic needs to increase its interoperability and product, I think Epic should prioritize product improvement to reduce customer flight risk. Epic gained a tremendous advantage by staying ahead of the trend to digitize, which positioned it well for the changes to the medical records industry since 2008. However, without further digital innovation, Epic lost its edge and is now relying on network effect to stay relevant and profitable. As we discussed in class during our Uber case, this makes Epic vulnerable to a potential negative “spiral of death.” It seems Epic’s system is sticky because it’s widely used but not interoperable. If Epic moves towards enabling interoperability first without improving its product, this could start a mass exodus of users from Epic to better EMR systems.
The point that “using Epic is easier than trying to piece together better options from various software vendors” is really key. I have looked at investing in many healthcare IT businesses, and the most prevalent theme in the EHR sector is consolidation to a single vendor across all modules. Hospitals don’t want and can’t afford to piece together best of breed solutions across practices–they all prefer to deal with a single provider out of simplicity, and Epic and Cerner have been the two biggest beneficiaries of this trend. The key difference between these two leaders is in their approach–Epic tends to build their modules in-house and is aggressively non-interoperative, consistent with Judy Faulkner’s style. Cerner on the other hand has been much more acquisitive and tends to be more open. At the same time, third party interoperability vendors are becoming more prevalent, and may ultimately be able to circumvent Epic’s fairly closed architecture. In the foreseeable future, though, I don’t see Epic losing any market share–if anything, they are continuing to gain.