The Digitization of Medical Records

It’s 2016, how can there still be paper medical records? For years Epic has been building an electronic database of patient health records but the hurdles of connecting hospitals around the world make this a slow and expensive process.
Anyone who has moved around a lot can attest to the fact that going to a doctor’s appointment in a new city feels like starting with a clean slate. It can be puzzling to think that you are responsible for providing each new doctor with your own medical history. Fortunately, the digitization of medical records is an effort that is well under way and should eventually lead to the health care industry being just as digitally connected as the rest of the world.
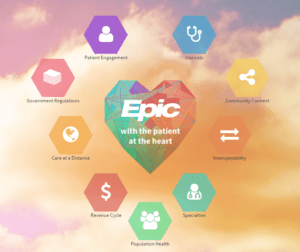
One of the largest companies in the Electronic Health Record (EHR) space is Epic, whose whole business model is based on building a digital health record data base to create value for the health care industry. Epic currently has EHRs for 190 million patients and can connect hospitals, clinics, specialists, hospice centers, and many other players to this information. Even a patient themselves can use the MyChart app to electronically access their record [1]. In addition to creating the software for specific hospitals and health networks, Epic also provides implementation services, training, and technical support [2].
As a patient, one can see the obvious upsides of convenient access and a collaborative network brought about with digital health records, but it is hard to imagine the scale of investment needed for hospitals to make this digitization change. Here in Massachusetts, Partners Healthcare is in the middle of a 2 year $1.2 Billion project to implement Epic across a network of 10 of their hospitals [3]. During this roll out it has been essential to provide enough training and support for everyone affected by the change. Despite the support provided by Partners and Epic, hospitals expect the initial learning curve to slow down their ability to serve patients before seeing an improvement. At Brigham and Women’s Hospital, in anticipation of the Epic implementation, they reduced their appointment volume for several days after switching to Epic; an adjustment with an opportunity costs of $15 Million [3]. While it may not be an easy or cheap undertaking, the hope is that better patient record access will lead to faster, more accurate care when walking into any of these hospitals.
After investing in the initial time and money to make the switch, the health care industry, from hospitals to patients, are hoping to eventually see lower costs. There are already some indications that EHR can reduce cost by reducing patient time at the hospital as described on Epic’s website: “A University of Michigan study of over 2,000 patients seen in the ED [emergency department] has shown…faster access to the information within Epic was associated with a 52 minute drop in visit time, as well as fewer repeat imaging orders and fewer admissions.” [4] Another opportunity is for providers to use this vast network of data to move towards value based costing which can improve quality of care and accuracy of charges for services [5].
In order to provide all the network benefits of having EHRs the hospitals need to all be connected to each other as well. This is an area where Epic and their competitors have drawn some criticism. The systems have differences that prevent interoperation which splits the EHR network and limits its capability to succeed [6]. In the private sector, the implementation of these EHR systems is considered “a strategic resource” [6] and critics believe that Epic is purposefully preventing the ability to share data between competitor systems [7].
Epic needs to realize that their value proposition to their customers becomes less valuable if they are not willing to connect their database with those of competitors’. Although Epic may be hesitant to work with competitors, their next step must be to find and execute a connection between the various EHR systems to create a complete network. If they can find a way to connect the patient data without compromising their system features they should see a higher willingness to adapt Epic across hospitals and health networks which will be a real growth opportunity for them. More adaptations will lead to an even larger network which will drive the cycle of the remaining hospitals wanting to adapt to EHR as well.
Epic is certainly providing value and improvements to the health care industry by offering these digitization and network creation services, but it is now up to them to put the importance of a comprehensive network at the top of their priority list.
(733 words)
- Epic Systems Corporation, http://www.epic.com/about , accessed November 2016.
- Epic Systems Corporation, http://www.epic.com/services , accessed November 2016.
- McCluskey, Priyanka Dayal, “Partners’ $1.2b patient data system seen as key to future”, Boston Globe, June 1, 2015, https://www.bostonglobe.com/business/2015/05/31/partners-launches-billion-electronic-health-records-system/oo4nJJW2rQyfWUWQlvydkK/story.html , accessed November 2016.
- Epic Systems Corporation, “Care Everywhere Shortens ED Visits by Nearly One Hour”, September 19, 2016, http://www.epic.com/epic/post/2335 , accessed November 2016.
- Oluwadamilola, Fayanju M., Tinisha L. Mayo, Tracy E. Spinks, Seohyun Lee, Carlos H. Barcenas, Benjamin D. Smith, Sharon H. Giordano, Rosa F. Hwang, Richard A. Ehlers, Jesse C. Selber, Ronald Walters, Debu Tripathy, Kelly K. Hunt, Thomas A. Buchholz, Thomas W. Feeley, and Henry M. Kuerer. “Value-Based Breast Cancer Care: A Multidisciplinary Approach for Defining Patient-Centered Outcomes.”Annals of Surgical Oncology 23, no. 8 (August 2016). (Published online early, March 15, 2016.), http://www.hbs.edu/faculty/Pages/item.aspx?num=50865 , accessed November 2016.
- Kohil, Rajiv and Swee-Lin Tan, Sharon, “Electronic Health Records: How Can IS Researchers Contribute to Transforming Healthcare?”, Management Information Systems Quarterly 40, no. 3 (September 2016). Business Source Complete, EBSCO, accessed November 2016.
- Creswell, Julie, “Doctors Find Barriers to Sharing Digital Medical Records,” New York Times, September 30, 2014, http://www.nytimes.com/2014/10/01/business/digital-medical-records-become-common-but-sharing-remains-challenging.html?_r=1 , accessed November 2016.
Picture Sources:
[7], [2], and http://tinyurl.com/zpfau5k




MIM,
As someone who had to go to three doctor appointments prior to HBS to collect my medical records and get additional vaccinations when the papers could not all be tracked down, I love the idea of digital medical records. However, one concern comes to mind — information security. I recognize that security is an issue with paper records (properly locked drawers and filed papers), and the AMA is already very focused on ensuring appropriate access for doctors or administrators (http://journalofethics.ama-assn.org/2012/09/stas1-1209.html), but I think we need to be concerned about connecting hospital networks. If one hospital in the Epic network gets breached, I as a patient would want assurance that the entire system of patient data is not exposed to hackers.
This is a perfect example of huge benefits from advancing into the digital age, but also tremendous risks to the privacy of individuals.
I share Cara’s concern about information security – it is a tremendous issue and hospitals are overall not great places when it comes to secure IT systems.
One tremendous benefit of Epic to the healthcare system as a whole (not just to an individual hospital/patient) is the data that these program generate. Researchers in healthcare have used insurance claims data to answer some questions, but also want more detailed clinical data that hospitals have. Historically, getting this data was manual and very institution-specific or required a parallel data collection process (as in clinical trials).
Epic is collecting tremendous amounts of data from hospitals which could be de-identified, aggregated, and used to meaningfully improve care quality and conduct retrospective studies. There are some early initiatives to do so – http://healthitanalytics.com/news/qpid-epic-ehr-combine-for-big-data-analytics-at-partners-health is an example. However, for the most part Epic is quite protective of that data and unwilling to share it with outside researchers…which is a shame.
Another point about how EMR’s bring “faster, more accurate care when walking into any of these hospitals” is that EMR’s have a tremendous power to reduce medication errors. A 2013 study estimates that about 400’000 patients die in hospitals each year due to preventable harm, many of them because medication was administered incorrectly or not at all (http://journals.lww.com/journalpatientsafety/Fulltext/2013/09000/A_New,_Evidence_based_Estimate_of_Patient_Harms.2.aspx).
Sophisticated electronic medical records require nurses and other healthcare providers to enter doses and medications administered to patients and, hence, open entirely new opportunities to secure that medication is administered correctly. Barcode scanners that feed into the EMR’s could ensure that the correct medication is administered and alarms could go off if a patient does not receive their medication in time. Additionally, in the event that patients take harm from medication errors, EMR’s provide more possibilities to identify root causes and systemic patterns given the large amount of data and its easy comparability.
I worked with Epic quite a bit in the past. Whilst I think they make incredible products, they have also garnered a lot of power in the industry and have used that power to further their own interests. Most of the time, people are okay with that, but when you are talking about things like healthcare, it invokes different emotions, rightly or wrongly.
It is possible to connect existing (seemingly incompatible) systems to share data, but requires interface engines in between to translate into the proprietary data schemas. These engines are processing-intensive though and it makes much more sense to focus on future data and ensuring it meets HL7 standards to ensure the easy transfer of data.
To the security points above, the concerns are very real, but they are also real for finance, education, government etc. States take different tacts for permission and this is one of the biggest bottlenecks to moving towards interoperability.