Roll Back Malaria: How Climate Change Is Affecting the Fight Against Malaria

Since becoming the focus of one of the WHO’s 8 Millennium Development Goals, malaria rates have rapidly declined. Will climate change threaten to reverse that trend?
The Roll Back Malaria Partnership (RBM), a collaboration between WHO, UNICEF, UNDP, and the World Bank to develop a global, coordinated anti-malaria effort, is now facing an additional obstacle to its goal of ending the malaria epidemic: climate change.
Malaria and Climate Change

Malaria is a life-threatening vector-borne infectious disease caused by parasitic protozoa; in 2015, there were 214 million cases of malaria worldwide. [1] Its incidence is highly correlated with the number and lifecycle of mosquitoes, which transmit the disease. Weather conditions such as rainfall, temperature, and humidity are known to affect survival of mosquitoes and length of the transmission season. Rising mean temperatures in particular have been shown to allow for increasing populations of mosquitoes in previously unexposed regions. [2]
The World Health Organization (WHO) and the World Meteorological Organization have recognized malaria as a key health issue that will be adversely affected by climate change, citing studies that suggest temperature increases of 2 to 3 degrees Celsius will place an additional several hundred million individuals at risk of contracting malaria. [3] A separate report published by the World Bank found that by 2050, changes in mean temperatures will result in a 50 percent increase in malaria transmission probability in regions in South America, Sub-Saharan Africa, and China. [4]
However, not all stakeholders agree that climate change will significantly alter the global impact of malaria. Researchers behind a study published in Nature in 2010 developed models to predict the impact of rising global temperatures on malaria transmission while taking into account the countering effect of continued global economic development and intervention, and argued that there would actually be a net reduction in malaria transmission. [5] Inappropriately shifting excess funds towards anti-malarial efforts due to misguided concerns around climate change would not without consequences, as these resources would likely have been diverted from other critical health issues.
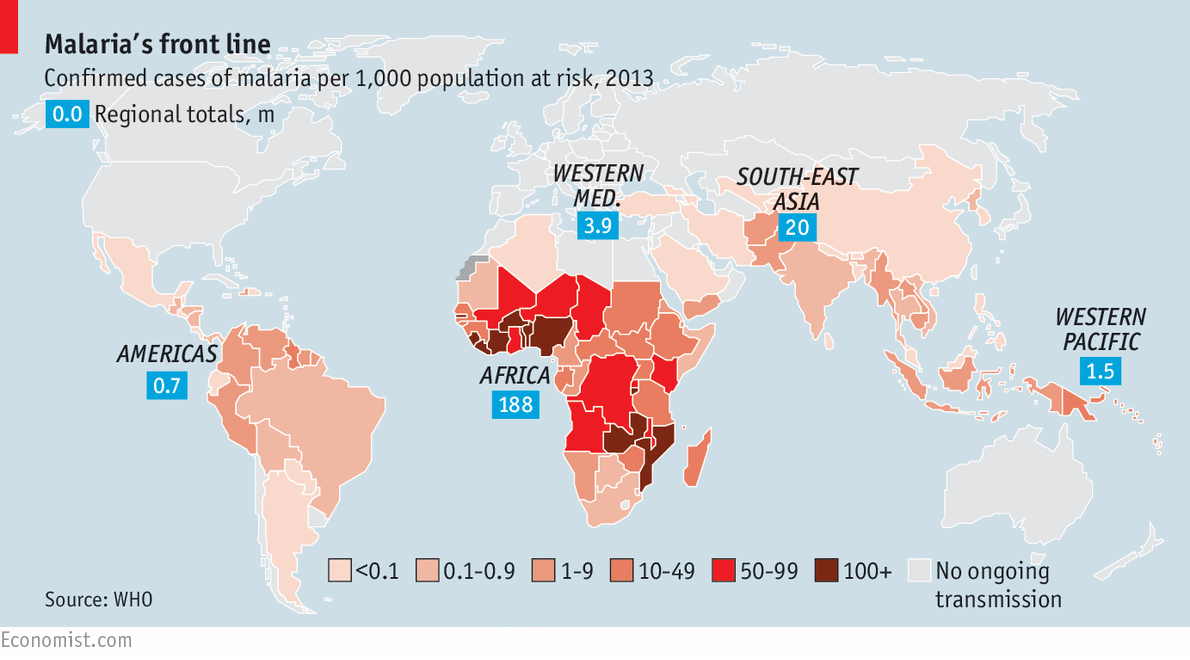 Worldwide malaria incidence, 2013. (WHO)
Worldwide malaria incidence, 2013. (WHO)
Updates to the Playbook: RBM’s Response to the Changing Landscape
In order to address the potential threat of climate change, the Roll Back Malaria Partnership developed an updated Global Malaria Action Plan with dedicated processes in place for measuring and mitigating against effects of climate change. [6] Specifically, the organization:
- highlighted the need to develop alliances with global and local environmental partners, such as national meteorological agencies
- called for identification of alternative sources of funding to meet increased future need, including funds set aside for climate change adaptation
- encouraged national programs to similarly adapt their malaria initiatives to address the potential impact of climate change
- recommended the development of data-gathering mechanisms to further surveillance and research on the link between climate conditions and malaria incidence
As an example, an early warning system has been developed in Botswana that combines a seasonal rainfall forecast with malaria surveillance data to predict incidence rates and reduce the lead time on a public health response. [6] Similar projects have been carried out in Sri Lanka and Ghana in an attempt to better forecast malaria trends and deploy appropriate interventions. [6]
Moving Towards a Malaria-Free Future
In addition to these efforts, the Roll Back Malaria partnership could take several further steps towards addressing the impact of climate change on malaria.
First, the partnership should work closely with and establish recommendations for key financiers, such as the Global Fund, the largest sponsor of malaria programs worldwide. [7] Many funders have yet to develop clear strategies for communicating the increased funding need that could result from climate change; Roll Back Malaria can play a role in supporting these efforts with the significant body of research it has assembled across its global efforts.
Second, Roll Back Malaria should proactively work with regions that were previously free of malaria-carrying mosquito species but are now predicted to be at risk within the next several decades. These regions are unexperienced in handling malaria epidemics and additionally are more susceptible to severe epidemics given the absence of adaptive immunity amongst the local population.
Third, Roll Back Malaria should focus on developing sustainable infrastructure for deploying interventions, such as delivering mosquito nets and anti-malarial therapeutics to difficult to access areas and populations. This strategy would mitigate against the potential risk that the global impact of climate change on malaria transmission is smaller than expected. Unlike funding spent on new drug development, for example, investment in infrastructure can be redeployed to address other emerging global health issues, thereby representing a sustainable investment in human health and welfare.
Malaria is just one amongst many examples of how global health will be affected by climate change. How can the WHO and partner organizations like RBM best prepare for these changes in the face of uncertain impact and limited resources? What are the costs of overestimating or underestimating climate-related risk? (781 words)
[1] World Health Organization, “Malaria Factsheet,” April 2016, [http://www.who.int/mediacentre/factsheets/fs094/en/], accessed November 2016.
[2] AT Peterson, “Shifting suitability for malaria vectors across Africa with warming climates,” BMC Infec Dis 9;59, 2009, p. 59.
[3] World Meteorological Organization & World Health Organization, “Factsheet #2: Climate information for protecting human health (2009),” September 2009, [http://www.who.int/globalchange/mediacentre/ events/2011/wcc3_factsheet2_health_en.pdf], accessed November 2016.
[4] The Potsdam Institute for Climate Impact Research and Climate Analytics, “Turn-down the Heat – Why a 4 Degree Warmer World Must be Avoided,” International Bank for Reconstruction and Development and World Bank, November 2012.
[5] Peter Gething, “Climate change and the global malarial recession,” Nature 465, 2010, p.342-46.
[6] Roll Back Malaria Partnership, “Action and Investment To Defeat Malaria: 2016-2030 For a Malaria-Free World,” World Health Organization, 2015.
[7] The Global Fund, “Overview,” 2016, [http://www.theglobalfund.org/en/overview/], accessed November 2016.



Thanks for the insightful article! I wonder what the impact of shifting funding in countries affected by Malaria from things such as infrastructure to healthcare will be. While health is arguably a higher priority than infrastructure the overall net impact on countries will be negative as a result of increasing malaria. International organisations need to shift their priorities of which countries are in most need and allocate funding accordingly.
Another issue to consider is that with rising temperatures many other tropical diseases (like dengue fever) will thrive in more countries. Are there diseases that are currently ‘under control’ but might escalate as more countries are affected?
This post clearly outlines the potential risk of climate change on malaria. The post also outlines some current and future steps towards lowering the risk, including warning systems, mosquito nets, funding and infrastructure to help fight epidemics, etc. When is the time to turn to science and engineering? An extremely controversial area of science with huge potential in this space is gene drive systems. This concept was explored by Heidi Ledford & Ewen Callaway in an article published in Nature in 2015. As described in the article, mosquitoes can be genetically engineered to resist the parasite causing malaria and CRISPR Cas9 technology can be utilized to ensure the genetically engineered components are inserted into both chromosomes and propagated through populations via reproduction (1). This type of engineering could provide massive resistance to mosquito-carried illnesses as climate change increases the incidence and risk. When is the right time to turn to gene drive type technologies? As gene drive has the potential to change entire species rapidly, is this too risk to employ, even if it can save lives? Will we ever begin engineering our ecosystems in such a dramatic fashion?
Source:
(1) Ledford, Heidi and Ewen Callaway, “Gene drive’ mosquitoes engineered to fight malaria”, Nature, November 23, 2015, http://www.nature.com/news/gene-drive-mosquitoes-engineered-to-fight-malaria-1.18858, accessed November 2016.
Ginger, thanks for a very helpful article! Given the potential climate change has to increase other diseases spread by mosquitoes – from dengue fever (as Stefan mentions above) to West Nile or chikungunya[1] – this could be a huge problem.
I am curious about why you think investing infrastructure would necessarily be better for Roll Back Malaria than investing in new drug development. I would argue that something like what the Gates Foundation is doing in trying to develop a vaccine or drug for complete cure and prevention[2] could have just as much impact, if not more. Even if the projected growth in malaria does not take place, we are still far enough away from worldwide eradication that such drugs would surely have tremendous positive impact. In addition, since RMB is focused on malaria and other organizations are already working to improve healthcare infrastructure, I am not convinced that it would be the best to overindex on step three just because the benefits could be realized by other health initiatives.
[1] Molly M. Ginty, “Climate Change Bites”, Natural Resources Defense Council, https://www.nrdc.org/stories/climate-change-bites, accessed November 2016.
[2] Bill & Melinda Gates Foundation, “Malaria: Strategy Overview”, http://www.gatesfoundation.org/What-We-Do/Global-Health/Malaria, accessed November 2016.
I think that thinking about climate change in the framework of healthcare is extremely important, so thank you for discussing this!
I agree with most of the comments above about the third option. Although on the short-run investing in infrastructure may be less costly incase the effect of climate change on malaria is small, I see that as an argument to just cut-to-the-chase and invest more to find a cure. I also like the idea proposed by Dean, though. My understanding of that research is that it is far too early for us to really understand the effects of that degree of genetic modification, especially on that scale. That being said, I think it is a pathway that carries a lot of potential and more research should be done. RBM may want to consider funding some of the exploration into gene drive solutions as part of a long-term eradication strategy. I guess I’m torn between where investments should be allocated. Is there a way to split investments between drugs to cure malaria and technology that can eradicate it? Both seem equally important to me at this point in time and it could decrease the effects of wrongly over- or under- assuming the impact of climate change.
Very interesting post Ginger!
With respect to your third proposed intervention (i.e., developing sustainable infrastructure for deploying interventions) it is interesting to think about the supply chains necessary to get health commodities to the populations at risk, and the implications of climate change for those supply chains. In places where malaria has traditionally been an issue, delivering commodities such as bed nets or anti malarials could become significantly more complex (e.g., refrigeration issues as temperatures rise, access to rural villages via dirt roads which can be affected by extreme weather) — a significant investment could be made in preemptive upgrading of supply chains, utilizing innovative methods (e.g., drone delivery, piggybacking off of the coca cola supply chain). In places traditionally unaffected by malaria, where infrastructure is being built from the ground up, it could be much cheaper to plan resiliency into that infrastructure in the front end, rather than invest in it at a later point. An overall infrastructure upgrade could be a huge opportunity to embed knowledge into processes and build the capability of local actors as well. Hopefully the RBM coalition will take a thoughtful approach to holistic implementation!
Oh you must be a doctor! This is a fascinating read and I didn’t realize that there was ever a controversy around the appropriate level of capital allocation for malaria. I wonder how the Nature 2010 article came up with its figures around the expected development of malaria intervention technology and practices. Furthermore, I wonder if the same report had any opinion on what other worldwide maladies would provide the most bang for the buck when it comes to intervention investment. Do you have any opinion on whether or not there are other diseases out there that deserve more or less attention/investment as related to malaria?
Ginger, thanks for this informative post about a truly scary disease that is still too prevalent. I was saddened to see in your exhibit that malaria still affects more than 10% of the population in parts of the developing world. Regarding your first suggestion on next steps, I would think about how to advance solutions for malaria from financiers outside of the Global Fund. The Global Fund, like the Gates Foundation, is a partnership/foundation that provides grants every year but there are now biotechnology and healthcare focused venture capital firms that can contribute investment to this focus area. As an investor myself, I see a lot of opportunity for funders to communicate not just the social impact of funding climate change adaptation programs, but also the potential financial returns.
For example, an Israeli startup called Sight Diagnostics has raised $10mm of funding so far to use computer vision to recognize malaria parasites in blood samples and distinguish them from other diseases (http://www.geektime.com/2016/03/24/meet-the-israeli-startup-that-could-stomp-out-malaria-in-africa-and-india/). According to Crunchbase, both Emery Capital and OurCrowd invested in the company’s Series B and could be funds that are targeting investment into the emerging healthcare space (https://www.crunchbase.com/funding-round/98405adc0e28d8f2aa4c65dbe96f9148).
Very interesting article, Ginger! I would be curious to know your perspective on whether or not pharmaceutical companies can play a larger role in preventative care, versus the use of mosquito nets.