Is the Hospital Industry “Feeling Under the Weather”?

Partners Healthcare is adjusting for climate change through changing operational designs of hospitals, implementing sustainable programs, and raising awareness of patient impact from climate change.
What does Climate Change have to do with Hospitals?
What institution operates 24 hours a day on equipment, consuming 2.5 times the energy used in other sectors, emitting 56 million metric tons of carbon dioxide equivalents per year? [1] What is the same institution which serves the casualties related to climate change? The answer is the hospital. Partners Healthcare, a Boston-based, non-for-profit healthcare system that includes hospitals like Brigham and Women’s Hospital and Massachusetts’ General Hospital, is paving the way in incorporating climate change impacts in its top priority strategy.
How is Partners Healthcare Adapting?
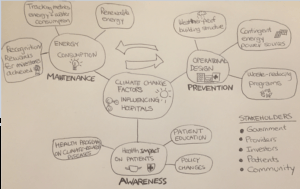
There are 3 main impacts on hospital systems which are impacted by climate change.
1. Operational design to deal with extreme weather events
Currently, the healthcare sector’s ability to respond to climate change is nascent in development. When Hurricane Sandy hit, Bellevue Hospital and NYU Langone Medical Center both had to evacuate because electric systems and backup generators were in the basement. It took more than two months before the hospital could operate again. Spaulding Rehabilitation Hospital, an affiliate of the Partners Healthcare system, instituted changes to its operation design to face the reality of climate change. One radical change is installing all electrical equipment on the roof of the facility rather than the basement. Other design changes include natural ventilation and on-site power generation, which allow the hospital to operate even during the weather events [2].
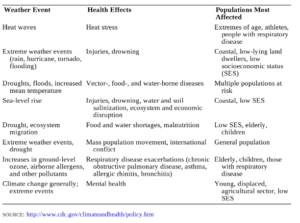
Source: See Endnote [3]
2. Sustainability in reducing energy usage and emissions
In the US, healthcare represents 18% of the of the entire GDP, and it is likely that it will increase in the future [4]. Given its enormous economic weight, the healthcare industry has enormous power in influencing the country in reducing fossil fuel usage. The US healthcare consumes 8% of the nation’s power and generates 8% of the country’s carbon dioxide emissions [5]. Hospitals release tons of regulated medical and hazardous wastes each day, some of which incinerated, into the air. Partners Healthcare is a founding member of the Healthier Hospital Initiative, which is a coalition of major healthcare systems across US to improve sustainability and safety in healthcare. Partners Healthcare’s primary goal is to reduce its energy consumption by 25% by 2020 [6]. A couple of initiatives include:
- On-site combined heat and power generation
- Renewable energy technologies
- Adoption of EPA’s Portfolio Manager Energy Star software for managing energy and water consumption
3. Anticipation for health impacts from climate change
Warmer global temperatures can cause more frequent extreme weather events, such as heat waves, droughts, floods and hurricanes. Health scientists claim that climate change will bring higher incidences of asthma, allergens, heat stress, viruses from increased weather conditions.
Recommendation
While Partners Healthcare is leading the way in many initiatives to mitigate risks involved with climate change, my recommendation is to integrate the 3 pillars of operational design, energy consumption, and patient impact into a holistic program. Furthermore, Partners Healthcare needs to consider the overall story to convey to its 5 key stakeholders: government, providers, investors, patients, and community.
Consider interconnecting operational design and energy consumption. When hospitals within the Partners Healthcare go through renovations or rebuilding, it is important to not only consider the physical construction, but also measuring system to track energy usage that is easy to use. It is important to stress that easy to track is key, as hospitals have many competing priorities in improving patient safety, speed, and quality. While adaptation to climate change might not realistically be in hospitals’ mission and vision statements, it should be outlined in the hospitals overall growth strategy. One tactical suggestion is running a monthly report on hospital usage, comparing to hospital standards. Based on metrics on energy reduction, Partners Healthcare should encourage policy makers to reward credits to hospitals.
Although energy reduction and patient outcomes may be hard to tie together, there are certain diseases such as asthma, allergens that are worsened as climate changes. Through education and advocacy, nurses and doctors are in a unique position to educate their patients about the public health impacts and be the spokespersons for energy policies to the government. Given their demanding schedules, these healthcare providers should play a more spokesperson role, and the hospital could partner with non-profit groups such as Asthma and Allergy Foundation of America and climate change forums to illustrate the long-term impact of climate change on health. Because the healthcare industry has such a large influence on market, a clear proposition would peak the attention of government and the investors.
Word Count: 780
Endnotes
Cover image source: Shutterstock
[1] Matthew J Eckelman, Jordi Sherman “Environmental Impacts of the U.S. Health Care System and Effects on Public Health,” PLoS ONE 11 (2016), accessed November 2016.
[2] Gary Cohen, “What does Climate Change Have to Do With Health Care?” Forbes.com, April 7, 2013, http://www.forbes.com/sites/skollworldforum/2013/04/07/what-does-climate-change-have-to-do-with-health-care/#79fa6b263e69, accessed November 2016.
[3] “Climate-Ready Spaulding Hospital Will Keep Boston Strong,” Adaptationstores.com, May 30, 2013, https://adaptationstories.com/2013/06/13/climate-ready-spaulding-hospital-will-keep-boston-strong/#more-266, accessed November 2016.
[4] Matthew J Eckelman, “Environmental Impacts of the U.S. Health Care System.”
[5] Ibid.
[6] “Partners Healthcare Hospitals Win National Health Care Environment Awards.” Partners.org, June 17, 2014, http://www.partners.org/Newsroom/Press-Releases/Practice-Greenhealth-Awards-2014.aspx, accessed November 2016.




Great insight on Partners Healthcare’s approach to addressing the pressing issue of climate change. You very nicely identify the 3 pillars of operational design, energy consumption, and patient impact, which serve as the corner stones of the Partner’s Healthcare climate change initiative. I agree a more holistic program will be beneficial.
I wholeheartedly agree that the government should issue hospitals carbon credits. At the end of (at least one) “food chain” in healthcare, their behavior can impact market behavior. Hospitals have a difficult time changing practices because of their complex systems and the high risk of compromising quality care. Their current needs are also (mainly) driven by the need to improve patient outcomes — and you see most innovative products in healthcare focused on this goal alone. While these outcomes need to remain priority, hospitals need to consume less energy and produce less waste. Hospitals should push healthcare businesses to innovate on products, including technology/machinery, to help hospitals reduce consumption. Carbon credits can provide hospitals with incentive to buy the newest products that help them achieve these results.
I thought this article did a great job of highlighting the challenges of climate change within the healthcare industry. As someone who is from New Jersey, I was able to see how local area hospitals were dealing with the impacts of extreme weather events in the aftermath of Hurricane Sandy (it was refreshing to read an article that brought this issue to light). Given how much hospitals rely on energy and its consumption in our country relative to other industries, I agree there must be more focus on sustainability. The challenge I see is the current ecosystem around rising healthcare costs and increased regulatory scrutiny as The Affordable Care Act continues to expand its reach nationwide. In controlling costs, it may be difficult to influence providers to adopt and invest in technologies that address some of these environmental issues. One of the local proposals I have heard about that is being considered is the use of solar panels on the roof to increase energy efficiency and decrease the reliance on other sources of energy (in addition to what you have mentioned in the article).
Another point I would like to highlight is that at healthcare providers such as Spaulding Rehabilitation Center, the use of treadmill and other exercise equipment (which are quite plentiful in these types of institutions) have the ability to generate and supply energy to the hospital that not only reduces operating costs but also represents a more environmentally-friendly solution to reducing energy consumption. In addition, because hospitals are high foot-trafficked areas, there is new technology that is capturing the impact of people’s footsteps in generating energy. From a disaster recovery perspective, these solutions represent sources of energy that are self-supplied and outside of the normal grid, and therefore, they are not susceptible to extreme weather conditions and other outside disruptions.
Thanks for the great post – it gave me a lot of insight into an industry that I am not that familiar with but is a heavy contributor to emissions. The survey of the industry and its relevance to climate change was extremely helpful. I especially liked your recommendations. Having an integrated program of operational design, energy consumption and patient outcomes is exactly what hospitals should be doing. Your ideas about usage transparency being part of the design is something the hospitals of tomorrow should adopt.
In regards to your point about the difficulty linking patient outcomes to energy reduction, I agree with you but also think there’s a great opportunity here. You mentioned one example of the changing prevalence of certain diseases and that is definitely true. In addition, I think designing a hospital with greater energy usage transparency and sensing / monitoring overall would contribute to better patient outcomes. Hospitals would have a better sense for the utilization, traffic or energy consumption across their departments which would enable more efficient planning. This could perhaps optimize labor and materials resources (or reduce error) which could improve patient outcomes. Further, this infrastructure of sensors could perhaps be used to better monitor or track patients, their environment and state of health during their stay at the hospital. There seems to be an opportunity within hospitals to align “greener” solutions with better outcomes.
Thank you for the insightful article. I was particularly interested by your suggestion of rewarding credits based on healthcare consumption. I think that this is a great idea and was thinking about how one might go about implementing this. With hospitals shifting to value-based healthcare models, where payments are linked to health outcomes, why can’t some payments also be linked to climate change? In this respect, perhaps a metric such as carbon emissions per hospital bed could be calculated, and based on this, certain payments made (or not made) to the hospital. This would clearly be controversial, but would certainly be a way of attempting to align incentives. Perhaps the credits could form the basis of certain tax credits – a solution likely to be more palatable than changing the way medicare and medicaid reimburse hospitals. As you mentioned, hospitals are a great carbon emitter, and helping them make not just their patients, but also the climate healthier should be a key priority.