Healthcare Social Networks: Can Crowdsourcing Patient-Reported Data Improve Outcomes?
In the United States, fifteen new cases of ALS are discovered every day, an estimated 1 million people suffer from multiple sclerosis, and an estimated additional 1 million people suffer from Parkinson’s disease. [1] These are the three main disease categories that PatientsLikeMe sought to address when they created an online platform for patients to share personal health information. Founded in 2004, PatientsLikeMe created a platform to crowdsource self-reported patient medical data to in an effort to 1) educate patients within disease-specific communities and empower them in their health journey and 2) advance the pace of medical research.
The Platform
PatientsLikeMe (PLM) has built an online social network for patients to exchange information within their disease-specific communities. Patients upload demographic information to their personal profile and share information on their disease, treatment plan, and symptoms. They can post and comment on articles, discuss new clinical trials, and direct message other patients for more in-depth conversations. Since 2004, the PLM network has grown to over 650,000 patients covering 2,800 different conditions. [2]
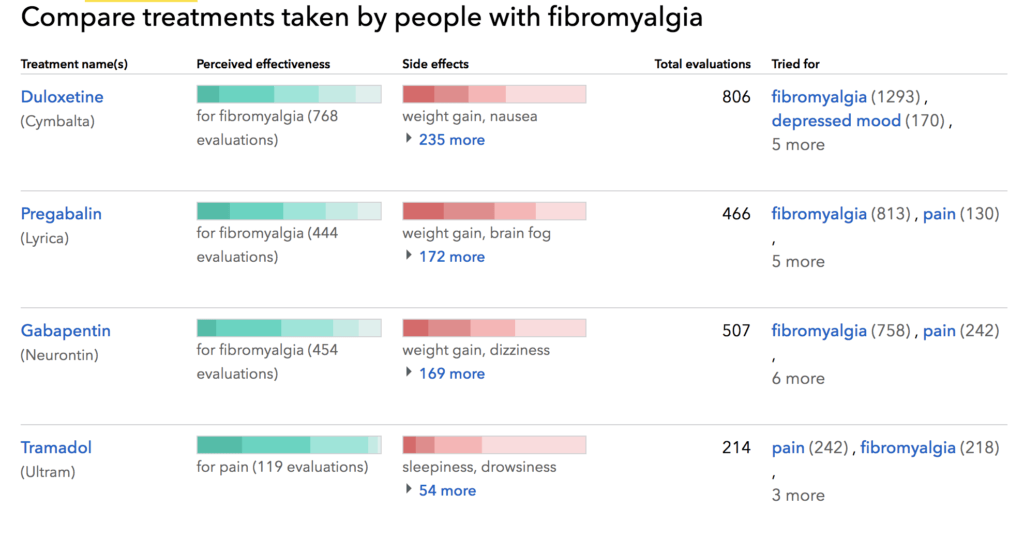
Figure 1: Visualization tools offered on PLM platform for patients with fibromyalgia. Patients can research information about the disease as well as compare treatment plans and reported side effects.
Educating and Empowering Patients – “Learn From Patients Like You”
The PLM platform offers an opportunity for patients to learn, connect, and own their health. Patients can review information to understand their best path given their condition and “Doctor Visit Templates” are available to empower patients to have more effective conversations with their doctor. [3] A 2010 study of PLM showed that 57% of patients found the site helpful for understanding treatment side effects and that 12% changed their physician as a result using the site. [4] In addition to providing information, PLM also provides an outlet for social and emotional relief. Patients can connect with a community of peers suffering from the same disease. In the same 2010 study, 41% of HIV patients and 22% of mood disorder patients reported community-specific benefits. [4]
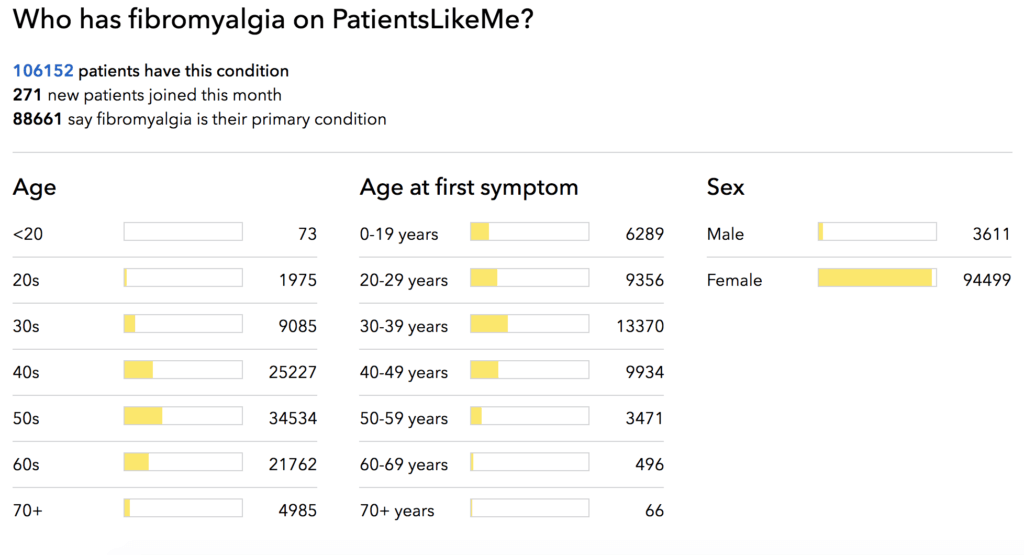
Figure 2. Patient biography on PLM platform.
Collecting Data to Advance Medical Research – “We’re more than a disease. Together, we’re the answer”
In creating a space for information-sharing, PLM has been able to collect large amounts of data and share them with 80 plus partners spanning biotech, pharmaceutical, and research. [2] They have partnered with the Journal of Medical Internet Research on numerous occasions. In one instance, it was to study the impact of two drugs (amitriptyline and modafinil) on patients within 5 disease categories (multiple sclerosis, Parkinson’s disease, mood conditions, fibromyalgia/chronic fatigue syndrome, and amyotrophic lateral sclerosis). [5] More recently, PLM data was used to observe the patient perspective on neuromyelitis optica spectrum disorders. [6]
A core competency in this process is PLM’s ability to de-identify patient information and convert it into structured, medically-accepted data. In 2018, an evaluative study showed that 97.09% of PLM-assigned codes, generated from their patient reported database, were compatible with FDA coding requirements. [7] This suggests that PLM reported data is reliably being converted into medically-accepted data. Managing this process and increasing coding reliability will continue to be essential to PLM’s model.
Open Questions
Crowdsourcing patient-data to improve the patient experience and accelerate medical research continues to generate enthusiasm within the healthcare community. Just last week, FDA Commissioner Dr. Scott Gottlieb announced that the FDA is launching a new app to gather patient-reported data for clinical trials. [8] PLM has built a strong platform to benefit from this trend, but there are some important questions that still need to be addressed:
- Can PLM overcome patient and population bias and leverage data to make meaningful medical advances?
- Patient bias – patients may report data incorrectly when submitting information.
- Population bias – PLM might be attracting patients that are not representative of the underlying population
- While patient reported data research is significantly less expensive than traditional clinical trials, it seems more appropriate as a supplement to clinical trials rather than as an alternative.
- Is PLM doing enough to help patients get better?
- Interactions are solely between patients. Should PLM incorporate advice from medical professionals? Should they leverage their database to identify highly skilled doctors and match them with patients?
References
[1] http://www.alsa.org/; www.nationalmssociety.org and http://www.parkinson.org
[2] https://www.patientslikeme.com/
[3] Brubaker, Jed; Lustig, Caitlin and Hayes, Gillian. “PatientsLikeMe: Empowerment and Representation in a Patient-Centered Social Network”. Semantic Scholar. 2009. http://www.gillianhayes.com/wp-content/uploads/2011/01/CnP11_PatientsLikeme.pdf, accessed November 2018.
[4] Wicks, Paul; Massagli, Michael; Frost, Jeana; Brownstein, Catherine; Okun, Sally; Vaughan, Timothy; Bradley, Richard and Heywood, James. “Sharing health data for better outcomes on PatientsLikeMe”. Journal of Medical Internet Research. June 14, 2010. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2956230/, accessed November 2018.
[5] Frost, Jeana; Okun, Sally; Vaughan, Timothy; Heywood, James and Wicks, Paul. “Patient-reported Outcomes as a Source of Evidence in Off-Label Prescribing: Analysis of Data from PatientsLikeMe”. Journal of Medical Internet Research. January 21, 2011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221356/, accessed November 2018.
[6] Eaneff, Stephanie; Wang, Victor; Hanger, Morgan; Levy, Michael; Mealy, Maureen; Brandt, Alexander; Eek, Daniel; Ratchford, John; Nyberg, Fredrik; Goodall, Jonathan and Wicks, Paul. “Patient perspectives on neuromyelitis optica spectrum disorders: Data from the PatientsLikeMe online community”. Multiple Sclerosis and Related Disorders Journal. October 2017. https://www.msard-journal.com/article/S2211-0348(17)30164-5/fulltext, accessed November 2018.
[7] Brajovic, Sonja; Blaser, David; Zisk, Meaghan; Caligtan, Christine; Okun, Sally; Hall, Marni and Pamer, Carol. “Validating a Framework for Coding Patient-Reporting Health Information to the Medical Dictionary for Regulatory Activities Technology: An Evaluative Study”. Journal of Medical Internet Research. August 18, 2018. https://medinform.jmir.org/2018/3/e42/, accessed November 2018.
[8] Arndt, Rachel. “FDA releases open-source app to collect patient-reported data”. Modern Healthcare. November 7, 2018. https://www.modernhealthcare.com/article/20181107/NEWS/181109936?mc_cid=cbc74122a0&mc_eid=04b2d4daeb, accessed November 2018.



I agree with your concerns about patient and population bias especially because this is sensitive medical data that can impact how a patient seeks treatment. There wasn’t any mention of any data governance or controls that PLM has implemented to attempt to protect against false data. Did you think about any type of review system or verification process that each submission would have to go through? Another concern regarding data is the input and formatting. The platform is only effective if all users input their data in a standardized format.
The most valuable piece of Patients Like Me seems to be the communities that it has built for individuals coping with their condition. It seems that their success in using this data to help diagnose conditions and advance treatment is limited. How might this patient-reported data be better synced with other sources of data, such as medical records or genetic information (e.g. 23andMe results) and if synced with these other data sources, would that provided more clarity to medical researchers?
This article represents a very interesting perspective on open innovation that combines the sharing economy with healthcare. While the sharing economy has disrupted the transportation industry as well as the hospitality industry (e.g., Uber and AirBnB), healthcare has taken a back seat until recently. [1] Patient health information is highly confidential and has various security concerns, both personal and legal. PLM’s process to de-identify patient information is critical for its operations and each patient’s trust that they will remain anonymous is required for this platform to scale.
While open expression of symptoms may be comforting, I am concerned with certain biases that patients have. For example, when people are not feeling well, they often seek support from their community. In this case, their community could be this online platform that may lead them to think they have certain symptoms or diseases that they, in fact, do not. When patients begin to self-diagnose, the practice of medicine breaks down completely. WebMD sees this with their diagnostic engine, which leads people to believe that they may have horrible diseases when it’s truly a simple cold. Health-based paranoia and hypochondriasis could manifest itself in this platform, which could lead to spreading fear rather than support.
[1] Leaders, O. T. (2017, June 22). Why Now Is The Time For Healthcare To Tap The Sharing Economy. Retrieved from https://hitconsultant.net/2017/06/22/healthcare-sharing-economy/
Because of the biases identified in your article, I’m equally skeptical about how meaningful the self-reported patient data is. I’m more worried about the self-reporting bias than population bias. Based on the screenshots you shared, it seems that the platform is collecting demographics data, which can be coupled with the patients data. If handled appropriately, the population bias may be mitigated. However, for self-reporting bias, it is harder to address. One way can be to develop machine learning algorithms to detect false data, e.g., patients who are reporting symptoms that are highly unlikely to happen together. Another way is to integrate medical records data, or partner with physicians to review and approve the reported data on the platform for the patients they see.
As for the value PLM creates, it should focus on the patient community. Thinking more about monetization, its patients community can also be ripe ground for identifying clinical trial targets.
This is a really interesting article and an even more interesting company. To answer your questions, I don’t think this should incorporate doctors and be more of a community applications. Yes, there is a risk of false information being spread, but I would imagine with so many stakeholders this wouldn’t spread too much. it would be no different than false information being spread between people in person. Second, I wouldn’t worry about falsely reported data. If this occurs, it would mostly be thrown out as spurious data on the scale that the data is being reported.
Your question as to whether or not PLM is doing enough to help patients get better is an interesting one. Most often, we consider treatment – especially for serious disease or illness – to be completely bound up in the medical treatment plan laid out by physicians. I would argue that a significant piece of the value proposition for PLM is that it is a community that provides information and recommendations without prescriptions. It offers information that can be individualized and empowerment that comes from being part of a group. I consider much of its value to be bound up in that it offers a network otherwise potentially inaccessible for a number of patients. That being said, I do believe PLM can leverage its database to identify highly skilled doctors and match them with patients through an OPT IN feature. That way, if a patient determines to change physicians, they can return to PLM to reduce the amount of time spent searching – especially in high stakes cases.