Electronic Health Records — when does data become too much?

Ever gone to the doctor and been unable to look your physician in the eye? Was it because you were embarrassed to say something or because he or she had his or her head down trying to type your entire response into the new Electronic Health Record? EHRs have ushered in a new era of modern medicine, but is it all good?
Do you remember going to the doctor’s office as a kid? I do. Between the shots, stickers, and “safety suckers” I remember my parents talking to the pediatrician while she furiously scribbled on pieces of paper. Fast forward 20 years and doctors are still furiously recording patient information, but the scribbling is replaced with clicks on a keyboard or swipes on an iPad as your doctor records your ailments and orders your medications directly through an electronic health record (EHR).
Meaningful use and the “digitalization of things” for the Health Care models.
With the adoption of the Affordable Care Act (ACA) in 2010, hospitals found themselves in a unique position. Among the new standards introduced was one of particular importance to the digitalization of Health Care—Meaningful use. Meaningful use standards were enacted to incentivize hospitals to switch from paper charting to an EHR. Designed to be implemented in 3 phases, Meaningful use meant “using certified EHR technology to:
- Improve quality, safety, efficiency, and reduce health disparities
- Engage patients and family
- Improve care coordination, and population and public health
- Maintain privacy and security of patient health information
Ultimately, it was hoped that compliance would result in:
- Better clinical outcomes
- Improved population health
- Increased transparency and efficiency
- Empowered individuals
- More robust research data on health systems
[2,4]
[2,4]
When the ACA was introduced, hospitals were functioning with two very distinct business models. Vanderbilt Medical Center in Nashville, TN, for example, needed to address two main issues for patients.
- “I need to know what the problem is, what is causing it and what I can do to correct it [1].”
And
- “Now that I know what needs to be done to fix my problem, I need it to be done effectively, affordably and conveniently [1].”
Operationally, being able to deliver on each of these models required medical institutions to function as two separate entities. The first, a “solution–shop,” necessitated a hospital have robust capabilities to diagnose and to develop treatment plans [1]. The second, an ability to carry out said treatment plan with specific processes and procedures [1].
Harnessing the EHR for operational efficiency
American physicians record 126 million out-patient clinic visits and 313 million inpatients days annually [6,]. In today’s medical setting, the EHR plays an integral role in physicians’ day-to-day tasks. The modern doctor spends as much time (or more) reviewing patient charts, recording data, and entering medication orders as he or she does interfacing with patients. But why is this?
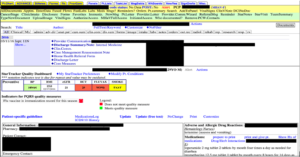
With the incorporation of the EHR, physicians now have a more robust mechanism to review patient charts. Take, for example, a patient transferred to Vanderbilt from an outside hospital for a severe asthma exacerbation. The first task for physicians, while the patient was in route, is to review previous notes, lab results, and medications—all included within the EHR (shown below). The EHR allows every physician in this patient’s care to review, simultaneously, real-time results. The critical care physician who manages the Intensive Care Unit, the pulmonologist seeing the patient upon arrival, and the Ear Nose and Throat doctor who may be consulted, can each see the patient’s most up-to-date information, and formulate their treatment initial plans based on data. Physicians can see what treatments have worked before and those that had not. This more robust EHR system merges hospitals’ business and operating models into parallel processes and combines all the patient data into a “searchable” database.
[10]
Does it actually work?
With the final phase of Meaningful use to be implemented in 2016, it is a good opportunity to stop and check if the digitalization of Health Care, particularly the incorporation of the EHR, has truly resulted in improvements. The Office of the National Coordinator for Health IT reports that 3x as many physicians believe an EHR prevented a potential medication error rather than caused one and greater than half of all physicians using EHRs were reminded to provide preventive care by their EHRs [3,5,8,9].
This picture, though, is not as rose colored as it seems as these same physicians reported longer working days, more time spent charting, and increased frustrations with the deluge of information presented to them through EHR platforms.
Fixing it going forward
Going forward, physicians will be faced with an ever-increasing onslaught of data and hospitals will have to find ways to cope with these new challenges introduced by the EHR. Potential solutions include the utilization of one standardized EHR platform throughout the country, as well as the leveraging of advanced computing technologies (like IBM’s Watson) to cull through and to make better use of unstructured medical data.
Overall, the digitalization of hospitals is an inevitability. The question, though, is how do we enable health care providers and patients to truly use the data they generate. (795 words)
Sources:
[1]http://www.forbes.com/2009/03/30/hospitals-healthcare-disruption-leadership-clayton-christensen-strategy-innovation.html
[2] https://www.cms.gov/eHealth/ListServ_RealWorldImpact_MeaningfulUse.html
[3] https://www.healthit.gov/providers-professionals/measuring-care-processes-and-outcomes
[4] https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives
[5] https://www.healthit.gov/sites/default/files/safetyqualitybrieffinal_sept2014_final.pdf
[6] National Hospital Ambulatory Medical Care Survey: 2011 Outpatient Department Summary Tables
[7] Summary Health Statistics: National Health Interview Survey, 2014
[8] The office of the National Coordinator for Health Information Technologies
[9] The office of the National Coordinator for Health Information Technologies: Physician-Reported Safety and Quality Impacts of Electronic Health Record Use
[10] Vanderbilt University Medical EHR



Hey fellow doc! Solid overview piece on EHR. A couple of comments: Is there any evidence that any doctor thinks EHR doesn’t increase efficiency? I currently don’t see how that argument could be made, so I’d be interested to see if you ran into that during your research. Of course, charting is tedious and keeps us away from home longer, but there is so much value in being able to access patient information quickly and thoroughly. To that point, I wonder if standardizing EHR nationwide would be possible because this move would inhibit fair competition in the market. For example, if Epic takes over community hospitals and academic medical centers, all the other EHR companies would have to battle over the private practices. But, for surgeons who consult in private practice but operate within larger hospitals, this division of EHR companies would be quite inefficient as they would have to switch between systems frequently even for the same patient. As for the actual practice of charting, Watson 2.0 needs to get on it ASAP so humans don’t need to input the patient data. Alternatively, scribes could fulfill that role everywhere to free up doctors’ time to spend actually interacting with patients.
As a patient I’ve definitely noticed the increasing levels of note taking. I think that Nelly-Ange’s point about finding a way to automate inputting data would be a huge step forward, but I’m curious whether privacy laws would allow conversations with patients to be listened to/recorded by a computer? There are so many rules out there.
I also think that setting up a standardized EHR would be helpful from a patient perspective. It can be challenging, particularly for those who move a lot, to keep on top of transferring medical records. I think it would create huge efficiencies if all records could be accessible on one portal that is visible to the patient and doctors that the patient has selected.
Great post, Graham! The integration of EHR’s into the medical community seems to be a tough challenge with many benefits, if done correctly. The integration strategy you outlined reminds me of a similar integration the Navy instituted over the past 10 years-the switch from paper charts to electronic navigation systems. Surprisingly, the outcomes you mentioned in your post (increased effectiveness but longer working hours) match very closely with my experience. While I experienced this integration first hand, I found the benefits obvious, but the changing of my behavior very difficult and time consuming. I wonder how long it will take to fully make the transition. Another concern I have about the nationwide standardization of electronic medical records is cybersecurity. I wonder about the implications of a nationwide medical record electronic database hack. Not only could personal identifiable information be released, but medical records could be potentially altered to adversely affect a targeted patient. While I think EHR’s are a net positive for society, there are definitely some risks that need to be addressed as we move forward. Thanks for the nice post!
Health data is particularly sensitive. We’ve recognized this, as a society, through laws like HIPAA. There’s always a risk associated to sensitive data. But I find it reassuring that my doctors are able to track my health over time and aren’t “flying blind” every time they meet me (especially if it’s a new doctor with each visit!).
As far as implementation is concerned, Nelly-Ange has me wondering — do you think that there is a business case for scribes to enter data into EHRs? At some of the Partners-affiliated locations that I’ve been to, I think they’ve shifted quite a bit of the data entry to a pre-visit with a nurse before a doctor comes into the room. Does that sound right to you?
Additionally, I’m wondering — do you have any sense for how all of this could change in a post-PPACA world? (i.e., if the law is “repealed and replaced”?) Do you think that, given the choice, any parts of the medical community would stop or slow the implementation of EHRs? I’d be curious. I imagine that collecting health information is fairly inevitable so it could be a shame to see the pace of development slow.
Thanks for the post, Graham. For the reasons described in your post and subsequent comments, it is clear that EHR has many benefits. A few thoughts regarding how technology might change the business model’s of companies working on the three stages of the EHR roll-out that you’ve identified:
1) Data Capture and Sharing – Could voice recognition technology be utilized to make medical documentation more efficient, similar to Nelly’s suggestion about scribes? Additionally, Google had a health initiative a few years ago in which Google users were encouraged to put their health data into Google Health. Unfortunately, however, Google shut down the project in 2013. Ideally, as Nicole mentioned, a centralized database with all patient information could provide providers with a better view of patients and enable them to provide better care.
2) Advance Clinical Processes – With the assistance of technology and evidenced-based insights into patient care, could processes be sufficiently improved and controlled so that lower-cost workers are able to provide the needed care? Similar to the clinical processes employed by Dr. Shetty in India. If lower-cost employees are empowered by technology to provide more technical care, it could help reduce overall healthcare costs.
3) Improved outcomes – In line with your comment about IBM’s Watson, could technology and artificial learning models help elucidate conditions or patterns for which a future health challenge is imminent. In such situations, providers could potentially use these insights to intervene or encourage lifestyle changes that may save a patient’s life.
Thanks for the post!
Great post Graham! As a patient, I’ve often wondered if it is possible to have an electronic health record that could travel with you as a patient and be transferred to your new doctors. It sounds like EHR transfers primarily occur within a hospital or if there is an official transfer that takes place. It seems like the ability for patients to have an ongoing EHR would allow doctors to spend less time re-entering data and have a more through record. I also find Nelly’s point about national standardization interesting, but I’m not sure how feasible it would be in the current healthcare climate.