Digital Diagnostics – The First Autonomous AI Healthcare Diagnostic

Exploring the game-changing impact of Digital Diagnostics in healthcare—how innovation meets accessibility, and AI transforms diagnostics. 🌐✨
In healthcare, AI is often used as an input into human decision-making and/or in improving processes, but rarely as an autonomous system. Examples of assistive AI abound: even within our class, we have seen VideaHealth’s dental disease detection and Watson’s cancer diagnosis tools. But these serve as inputs into dentists’ and oncologists’ decisions — no matter the accuracy, the final decision still lies with the human. Digital Diagnostics is revolutionary in that it is the first autonomous AI system to be cleared by the FDA to be able to provide a diagnostic decision.
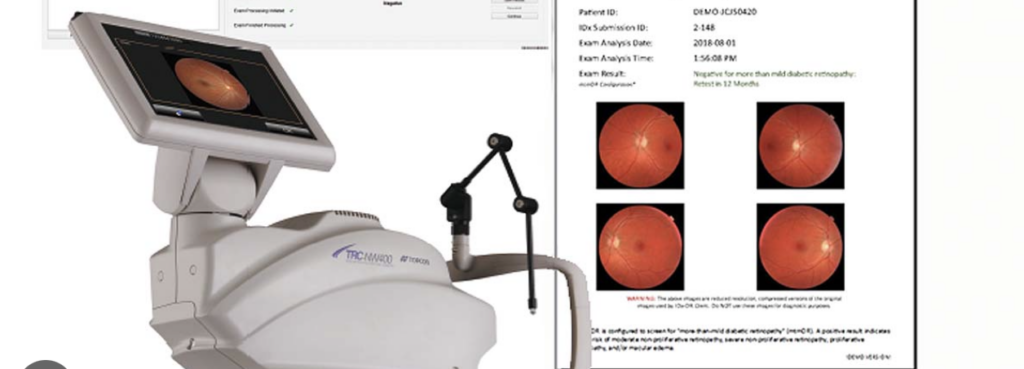
Digital Diagnostics utilises artificial intelligence (AI) to enhance the detection and management of diabetic retinopathy, a common eye disease that can lead to blindness. The company employs advanced AI algorithms to analyse digital images of the retina, providing valuable insights into the presence and severity of diabetic retinopathy. Rather than serving as an assistive system to ophthalmologists, Digital Diagnostic’s imaging hardware (and associated AI software) are installed in primary care physician offices, serving as a screening tool. If a patient receives a positive diagnosis, they can then be referred on to a specialist by their PCP. The AI system can efficiently screen large volumes of retinal images, automating the screening process and increasing access to care where previously a patient had to incur $150-200 to even get a consultation with an ophthalmologist. This is particularly beneficial in healthcare settings where there may be a shortage of ophthalmologists or other eye care specialists.
Creating Value – Improving the Productivity Gap
Digital Diagnostics set out to address the core issues plaguing the healthcare industry — the ever-increasing cost and persistent health inequity. Dr. Michael Abramoff, founder of Digital Diagnostics, identifies the root cause of these problems as the productivity gap in healthcare. Despite the widespread adoption of information technology, the industry has seen a decline in productivity over the last 50 years. This productivity gap has resulted in soaring healthcare costs, unequal distribution of healthcare, especially among minority and rural populations, and increasing difficulty in accessing timely medical care. The introduction of technologies like electronic health records (EHRs) has, in fact, made physicians and healthcare as a whole less productive.
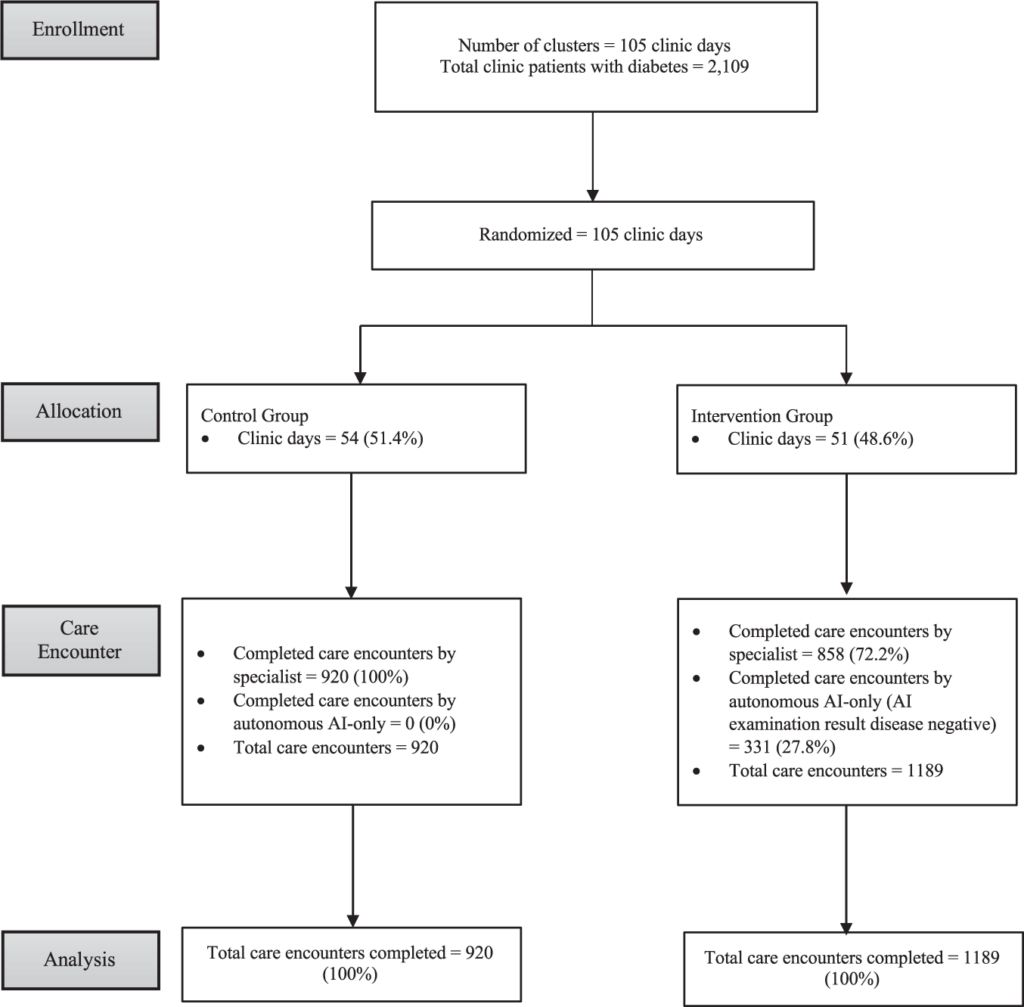
Digital Diagnostics proposes a paradigm shift — the adoption of autonomous AI in healthcare. The idea is to leverage AI technologies to automate healthcare tasks, especially in the realm of chronic diseases like diabetic retinopathy. The ultimate goal is to improve productivity not only by making individual tests faster, but by enhancing access, lowering costs, and increasing overall quality within the healthcare system. The autonomous AI system developed by Digital Diagnostics, known as IDx-DR, represents a concrete step towards addressing these challenges. IDx-DR autonomously diagnoses diabetic retinopathy and other diseases like macular edema. By enabling point-of-care diagnostics without the need for constant physician oversight, the technology not only speeds up the diagnostic process but also makes high-quality healthcare more accessible, equitable, and cost-effective. In their latest trial published in Nature Digital Medicine, they show that their system allowed specialists to focus their time on more complex patients, as well as reduced wait time to patients.
Capturing Value in a Complicated Industry
Digital Diagnostics faced an even more fundamental problem: in an industry where services are often paid for by insurers or governmental bodies, they needed to find a way to have their product be paid for. Individual patients and even physicians would not be the customers paying for their product. Their process was a long one — even after the FDA granted de novo authorization to the autonomous AI system after a pivotal trial addressing safety, equity, efficacy, and bias, they needed patient organizations, such as the American Diabetes Association, to support the use of autonomous AI for the diabetic retinal exam. Then, they got evidence-based medicine experts to update quality measures, and physician and provider organizations created a dedicated Current Procedural Terminology (CPT) code for the AI system. Government health programs, particularly the Centers for Medicare and Medicaid Services (CMS), finalised national values for reimbursement, emphasising transparency with Resource Based Relative Value Units (RVUs) at $45-$64 per exam.
As with all first-movers to a market, the pricing of autonomous AI diagnostic products is a tricky one. How do you price a product that effectively has zero marginal cost (to run an additional prediction)? Ideally, you would simply be able to provide access to screening technology to everyone. How do you align incentives to improve access to all on a reimbursement system that is coded at a price per exam? It might be better to move to a subscription model (e.g., physician pays a fixed cost to use the technology every month, rather than paying per scan), but the healthcare reimbursement system simply isn’t structured that way.
The financial model surrounding AI implementation poses critical questions about reimbursement codes and potential kickbacks. Addressing these concerns is vital for the sustainable growth of AI in healthcare. Moreover, understanding the referral patterns of high-risk patients and the decision-making process of primary care physicians becomes imperative in refining the triage system.
Opportunities for the Future
Looking ahead, Digital Diagnostics is poised to revolutionise how clinics approach early disease diagnosis. They stand to gain from “horizontally integrating” various diagnostic processes and offering a standardized platform for managing multiple touchpoints in early diagnosis. In the future, rather than contracting with many autonomous AI firms each specialising in their own disease recognitions, clinics can aspire to have a single, comprehensive platform that can seamlessly handle diverse early diagnosis diseases. This approach not only simplifies the management of diagnostic workflows but also enhances the overall quality of patient care. In being the first player in this space — and given their tight links to the FDA and to both academia and industry — Digital Diagnostics is at the forefront of shaping a future where healthcare professionals can navigate multiple diagnostic touchpoints effortlessly, ultimately leading to improved patient outcomes and a more efficient healthcare ecosystem.
—
Sources linked in text.



Interesting stuff. I wonder at what cost though doctors are willing to pay for efficiency? The incentives of the health care system reward doctors for frequent visits, and this model threatens to disrupt that. Also, I wonder how this technology will attempt to build trust with patients?
Super interesting! Where are they getting their data to get the flywheel going? Something like India Stack’s healthcare vertical seems ideal for this (although I realize that’s not their target market) since it facilitates collection of comprehensive healthcare data across the country. I’m also curious what degree of diverse data one requires for this? Will a certain population show different symptoms compared to others and thereby go undetected? How are they solving for that?
I see B2B SaaS as the closest model for pricing since it also isn’t cost based and has a similar parallel of “each additional task has zero marginal cost”
This was a great click down on how AI is potentially disrupting the health care industry. Do you have any data or thoughts on what level of accuracy the service would need to achieve consistently before people (patients or doctors) would become comfortable using it? Or is it such a cost and time saving innovation that people are willing to sacrifice some accuracy for the benefit of efficiency?
Hmm, if the AI is as accurate and independent as they claim, I wonder why they even need to be present at doctor’s offices…could users not just submit an image of their retina online (or through their webcam)? I imagine there might be some special lighting or other adjustments needed for the images, but as the models get better, I can see at-home AI health tools being truly revolutionary. Alternatively, as you mentioned that the marginal costs for each test is effectively $0, I think this could also be a great tool to have at schools, supermarkets, and churches (much like those blood pressure monitors), since healthcare can essentially be treated as a public good (and hopefully government backed).