UnitedHealth: Losing Ground to New Entrants

UnitedHealth group struggles to defend its core business from the new digital startups like Oscar Health and Bright Health
Health insurance value chain in the US has been in flux for the past decade, partly thanks to the political instability (think Obamacare vs. “Trumpcare”), and more importantly, due to significant technological advancements. Impact of digitization has been tremendous in closing the information gap between payers and providers as well as providers and patients – Electronic Medical Records (EMRs) systems facilitate information sharing amongst providers, digitalized billing platforms streamline processes and enable population health analytics, and telemedicine and other direct-to-consumer technologies empower patients to be more engaged in their care and expect higher levels of service, quality, and affordability1.
Oscar Health and Bright Health, two new entrants in the market have each raised $727M and $240M respectively, on the premise of disrupting health insurance by building a direct relationship with customers2,3. At the core, these new business models and others in the category leverage clinically integrated physician organizations to offer health insurance that is simple, friendly and affordable – shifting consumer mindset and their perspective of insurers from “a necessary evil” to a service they love4.
The emergence of these new business models is expected to have significant implications for traditional payers like UnitedHealth, shifting customer demand to lower cost, higher quality payers like Oscar Health and Bright Health while negatively impacting the bottom line due to the increased cost required to match the competitor’s service.
Source: CBInsight
UnitedHealth’s [marginal] digitization efforts
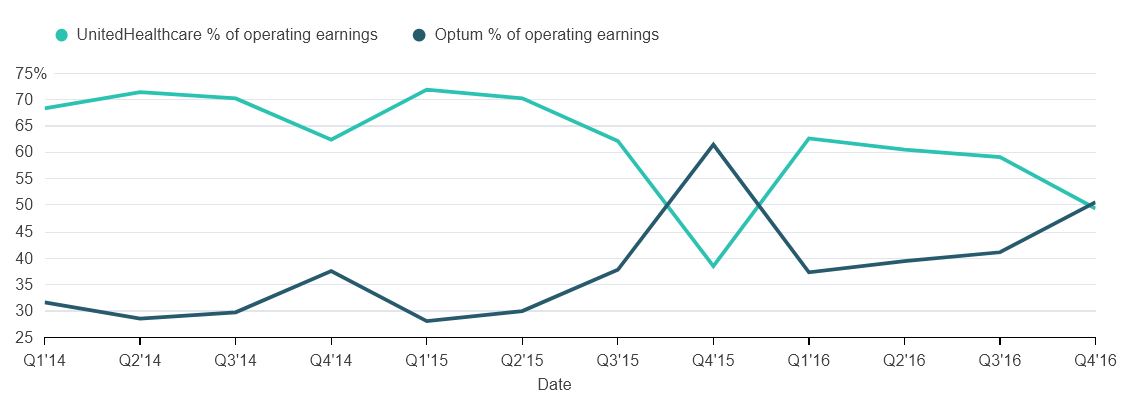
As the market leader and largest insurance provider in the US, UnitedHealth Group has sustained its dominance and “data supremacy” through significant investments and multiple acquisitions – forming a new subsidiary Optum, the largest healthcare IT company in the world by revenue5. Optum’s health data analytics, payment integrity, risk assessment and medical billing capabilities have proved effective and its performance was the highlight of 2016 for UnitedHealth, with earnings reaching over 50% of total operating earnings6.
Source: Bloomberg
Importantly UnitedHealth has been ahead of its other large, traditional competitors in adapting to the new paradigm shift, mainly through acquiring health data analytics companies to bridge some of the existing information gap – A few good examples of this are UnitedHealth’s acquisition of Axolotl, a Health Information Exchange (HIE) software and services provider, and Picis, a developer of Electronic Medical Records (EMR) for hospital emergency units. Later in 2013 UnitedHealth also acquired Humedica, a clinical data analytics vendor that enables providers to instantly access and compare medical record data changes across time and provider group – a true prize catch for UnitedHealth in its efforts to build on its profitable data empire and differentiate itself amongst other traditional, large competitors.
Despite Optum’s financial success, however, UnitedHealth has failed in leveraging its data empire to improve quality of care or affordability in meaningful ways – providing fertile ground for new entrants like Oscar Health and Bright Health to grow exponentially4.
Looking forward to [a bright] future
In 2016 alone, UnitedHealth’s revenues grew by $17B and reached $144B7. The company is growing at incredible pace, and investors remain optimistic about its growth path, as evidenced by its sustained share price increase despite overall industry turmoil. Moving forward to effectively maintain its market leadership, UnitedHealth should implement a long-term strategy that ensures the following:
- Integrate more directly with providers and health systems and therefore gain access to large sets of clinical data while reducing the pool of providers available to new entrants
- Invest significantly in mobile apps, telemedicine and concierge services to improve quality of care, customer satisfaction, and operational efficiency
- Consider launching company owned primary clinics, urgent care, and specialty care centers
UnitedHealth has already been experimenting with some of the above initiatives such as select telemedicine and preventive care programs to increase the quality of care but has achieved mixed results. The success of such programs, proven by many startups such as Oscar Health and Bright Health, require more than just monetary budget allocations and investments, and will only succeed if implemented in a fully integrated ecosystem where patients care journey is curated in a controlled setting fostering data transparency, and accountability. UnitedHealth is well positioned to leverage its existing relationships with customers and care providers to create such micro-ecosystems that are more regional and targeted by design and therefore can foster a more holistic and personal service to patients.
Looking forward, two key questions remain: can this disruptive and entrepreneurial strategy be implemented in a sustainable way at a large corporation like UnitedHealth? And if so, are management and shareholders incentivized to commit to this undertaking given the current broken healthcare system and political turmoil?
(751 words)
Works cited
[1] “The Innovation Health Care Really Needs: Help People Manage Their Own Health”. Harvard Business Review. October 30, 2017. Accessed November 10, 2017. 1. https://hbr.org/2017/10/the-innovation-health-care-really-needs-help-people-manage-their-own-health
[2] “Oscar Health | Crunchbase.” Crunchbase.com. Accessed November 10, 2017. 1. https://www.crunchbase.com/organization/oscar
[3] “Bright Health | Crunchbase.” Crunchbase.com. Accessed November 10, 2017. 1. https://www.crunchbase.com/organization/bright-health
[4] “Oscar Strategy Teardown: How The Health Insurer Is Beginning To Hedge Against Obamacare.” Cbinsight. October 26, 2017. Accessed November 10, 2017. 1. https://app.cbinsights.com/research/oscar-health-insurance-strategy-teardown-expert-intelligence/
[5] “Data battle: UnitedHealth deal is the latest move in industry shift”. Modern Healthcare. February 2, 2013. Accessed November 10, 2017. 1. http://www.modernhealthcare.com/article/20130202/MAGAZINE/302029973
[6] “UnitedHealth Has Trump Insurance”. Bloomberg. January 17, 2017. Access November 10, 2017. 1. https://www.bloomberg.com/gadfly/articles/2017-01-17/unitedhealth-secures-insurance-against-trump-uncertainty
[7] UnitedHealth Group. (2016). Form 10-K 2016. Retrieved from http://www.unitedhealthgroup.com/~/media/5D60EEEE258F4D2FA4BA765727C41D5C.ashx



Faraz, great article. It’s really interesting to read about how UHG is competing with newer entrants in the healthcare space (not unlike other sectors where startups are disrupting the status quo). It seems like they have been more successful than other large companies in “digitizing” although I think they have a ways to go. I think they need to keep utilizing M&A to compete with the new players on the block. Could they be a possible buyer for some of the main competitors in the industry? This would be an expensive, although potentially worthwhile, strategy for UHG.
I think the biggest question moving forward, as you mentioned, will be whether UHG can implement a disruptive mindset within the organization. This has to start from the top down and will require buy-in from the employees. It will be interesting to see what they do over the next 2-3 years as more entrants enter marketplace.
Faraz, this is really helpful. It’s interesting that United Health Care has used Clayton Christenen’s theory on disruptive innovation by setting up a subsidiary unit in Optum to help accelerate its innovation. As I understand it most of Optum’s revenue is generated from services, not from the payor / insurance side. Do you think that UHG can stand up a similar unit to Optum or Bright Health? Or is that not necessary for UHG to continue to be a key player in the insurance space.
Really enjoyed this piece, Faraz. Thanks for tacking such a broad and complex topic. I think this touches on a lot of key issues in healthcare, and one of those is the opportunity for better connectivity between different parts of the healthcare system. To the extent the new entrants are able to get this done, it’s fantastic and can lead to more personal, holistic treatment paradigms and lower costs as well. That said, health systems are working with highly customized health electronic health records and interoperability is quite a big burden.
Getting to your questions, the above makes me think that UnitedHealth is indeed well positioned to respond to the entrepreneurial value propositions. By leveraging it’s massive set of covered lives, investments towards systems interoperability should be much lower on a per-unit basis. Also, in today’s class we learned about the “flywheel” and “chicken & egg” dynamic in creating a market between customers and suppliers. Surely UnitedHealth’s massive customer base would offer a higher incentive for suppliers to invest in standardization (and this would of course cycle back to more value for customers).
Great piece Faraz! I agree that the future of medicine will be digitized but I, like you, wonder whether United can successfully compete in this new world given its structural disadvantages. The business was originally set up to serve a less technologically advanced market, and I’m not convinced they will be able to restructure in a way to successfully compete with cheaper, simpler new entrants over the long run. It will also be incredibly expensive to change. But luckily for United, they have the financial resources to attempt to make the transition.
In regards to your other question about whether United should attempt to digitize given the current healthcare policy uncertainty, I think they still have to. Even if healthcare policy has not caught up, digitization represents the future of healthcare.
Looking forward, two key questions remain: can this disruptive and entrepreneurial strategy be implemented in a sustainable way at a large corporation like UnitedHealth? And if so, are management and shareholders incentivized to commit to this undertaking given the current broken healthcare system and political turmoil?
Great read, Faraz! I think it is possible for large organizations to implement disruptive changes, though I do think it will be more difficult. After witnessing a hospital in the midst of implementing Epic software, I realized the large amount of orchestration it takes to implement such a change. There needs to be a clear timeline, regular town hall meetings, and outlining of goals and expectations. There also needs to be adequate support in the early phases of the transition to work out any issues as people get up to speed. However, it is certainly possible with the right amount of planning and motivation.
Personally, I doubted UHG’s ability to set up a entrepreneurial business unit within it’s legacy organization. They might have moved slower to the pace of change required to not get out competed by the start ups. However, in immediate juxtaposition to that hypothesis is the how big a portion of UHG’s revenues Optum makes up. They have a huge cache of experience and data and seem to be pulling it off.
However, they key unlock Oscar etc bring is changing the fundamental relationship with the patient has with their healthcare. I know UHG can get “digital” but I wonder if they can usher in a more efficient paradigm.
Thanks Faraz for a great analysis of an interesting problem. I think you do a great job of delineating the challenges UHG faces, both from a shifting eco-system as well as from new technology savvy entrants like Oscar and Bright. To your question on UHG’s ability to implement these changes at scale, I am not bullish. Part of the inherent problem is that the degree of integrations required with clinical partners (hospitals, physician groups, etc) are somewhat contrary to the way in which UHG has grown. As many large health insurance companies, UHG has developed scale via acquisition and, as such, has the difficulty of managing interoperability of technology systems and data platforms across its empire. This poses challenges as hospital systems try to merge or integrate platforms with UHG, relying on technology operations that are rooted in both regional subsidiaries as well as at the corporate parent.
Start-ups like Oscar and Bright will be able to accomplish this better at regional levels because they have recently built their tech stacks and have fewer platforms to consolidate. Given their regional focuses, they are able to focus resources on deeper integrations with partners in key markets. While it will be a long time until they can pose a risk to UHG at scale, similar to the disruptive innovation model referenced, they will be able to win share through incrementally better offerings in core markets, with their competitive threat growing over time.
Very interesting perspective on digitization, Faraz. I think the critical thing here is to note that (from personal experience) insurers have a hard time deploying new technologies within their ecosystem. And as we have seen from IBM Watson’s struggles [1], unlocking clinical data is even harder, especially from the EMR. I think you are right to mistrust the ability of UnitedHealth to deploy and adopt technology quickly.
However, I would also doubt the ability of Oscar and Bright Health to do this as well. Healthcare is slow, and companies like Oscar are burning money and unprofitable [2], so unless a company is in it for the long haul and can raise long-term capital, I’m unsure who will win.
Stockholders rarely invest in the long-term. Given the political uncertainty with the healthcare system, shareholders will probably not value new technology deployment as part of the stock price. However, given UnitedHealth is a behemoth and its divisions are rather opaque, they probably have a better chance of implementing something like this through a 10-15 year sustained effort (if value-based payments continue), than startup insurers who exist today.
To summarize, the future is bleak for technology in health insurance, but UnitedHealth has a better shot than young upstarts.
References:
[1] Freedman, D. (2017). What will it take for IBM’s Watson technology to stop being a dud in health care?. [online] MIT Technology Review. Available at: https://www.technologyreview.com/s/607965/a-reality-check-for-ibms-ai-ambitions/ [Accessed 1 Dec. 2017].
[2] Goldberg, D. (2017). Amid continuing losses, Oscar searches for the right strategy. [online] Politico PRO. Available at: https://www.politico.com/states/new-york/albany/story/2017/08/30/oscars-numbers-dont-yet-match-its-rhetoric-114220 [Accessed 1 Dec. 2017].