Santa Clara Valley Medical Center: Pioneering Spinal Cord Injury Care With Telemedicine

Santa Clara Valley Medical Center’s (SCVMC) Rehabilitation Center is creatively addressing the needs of vulnerable patients living with spinal cord injuries by digitizing healthcare through telemedicine.
Increasing External Pressures Affecting Patient’s Quality of Life
Spinal cord injuries (SCI) are catastrophic injuries that have permanently altered the lives of 282,000 U.S. citizens[1]. The consequences are far-reaching, causing subsequent paralysis, limited mobility, and secondary complications. These patients require time in rehabilitation centers to physically recover, psychologically adjust to their new state, and education in how to cope with these permanent changes.
Unfortunately, the health care industry is trending to reduce length of stay to cut costs, shortening rehabilitation length of stays from 98 days in the 1970s to 35 days today; this trend reduces the crucial time needed by patients to better manage their newfound disability and it increases the risks of secondary complications[1][2]. Approximately 30% of SCI patients are re-hospitalized one or more times in the year following their injury, wherein urinary tract infections and pressure ulcers are the leading causes[1]. These rehospitalizations are costly to all parties and possibly fatal for patients. Hospitals incur an average of $43,180 for each ulcer and these ulcers cause 17,000 lawsuits to be filed against hospitals annually. On the patient side, pressure ulcers cause 7 – 8% deaths of those of SCI patients[2][3].
Secondary conditions, such as pressure ulcers, are often preventable with the proper care, but it is difficult for SCI patients with low income or those living in rural areas to receive this specialized medical care[4]. Given the limited amount of organizations that have rehabilitation specialists, the commute for some rural disabled patients could take hours. Due to the time commitment, financial pressure, lack of mobility, and/or inflexible work hours, vulnerable patients are likely to delay diagnosis and treatment, further exacerbating the likelihood of secondary complications[5].
Remediating the Cost and Reach Issues with Telemedicine
To deal with the issues stated above, for decades the Santa Clara Valley Medical Center sent their SCI specialist out to rural areas 8-10 times a year to conduct outpatient clinics across Northern and Central California[4]. While this solution did provide relief for many patients, it is far from ideal. There are still issues regarding the infrequency of access, general lack of flexibility, and the costs of sending medical teams across California.
Recently, SCVMC has been exploring the possibilities of using telemedicine to address the shortcomings of their historic approach to the problem. By utilizing consumer technology, SCVMC is exploring the possibilities of managing secondary complications and improving overall quality of life (QoL) for individuals with SCI. There has been prior research that showed positive results in reducing stage II and stage IV ulcers when incorporating telemedicine to increase accessibility to patients (particularly those in rural areas)[6].
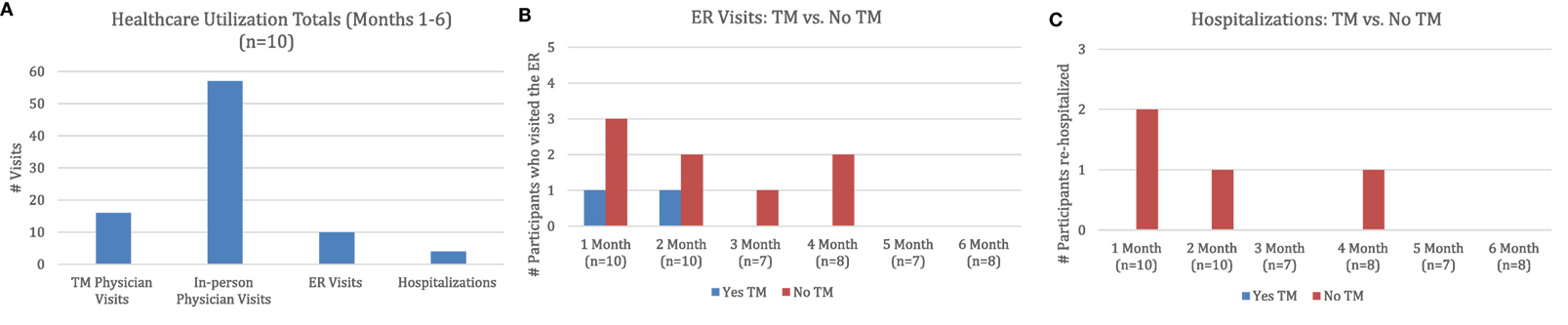
SCVMC began a study by supplying a small group of individuals with iPads and showing them how to schedule an appointment and have a live consultation via FaceTime; this research was the first known project to utilize iPads as a telemedicine entry-point[4]. The 6-month study concluded with a high patient satisfaction rate and enabled a more accessible method to transfer important information regarding the complications of living with SCI to patients. The hospital’s research suggests that there is a feasibility when using these types of tools to increase patient QoL and ideally these findings can be expanded to other areas in medicine.
Although the findings were positive, SCVMC has not publicly announced any definitive plans for the medium-term yet. This is understandable given the nature of the healthcare industry; any incremental changes to patient care needs to be meticulously studied and approached with caution.
Further Suggestions for SCVMC Rehab Center
I fundamentally agree that there is significant value to be added in advancing patient care by digitally connected patients directly to the hospital’s resources. I believe they can catalyze this change by focusing on the cost benefits. The current research SCVMC has done is focused on patient QoL, and while that is extremely important, there can be a larger push for change by the entire organization if their research stated the financial aspects of telemedicine.
By utilizing time-driven activity-based costing on preventable rehospitalizations, the hospital can have a better side-by-side comparison of the cost difference between telemedicine and the status quo. SCVMC should undertake a longitudinal study that shows the difference in absolute costs due to the decreases in secondary complications.
Given the greater accessibility and decreased variability for patients access to their doctors, they should also study telemedicine’s effect on missed appointments (which is estimated to cost the U.S. healthcare system $150 billion a year[7]).
Questions?
By moving appointments from in-person to online, how will SCVMC ensure that these consultations achieve parity in quality?
Should this program be widely available for all patients, or those that have exceptional difficulties reaching the hospital?
Word Count: 775
Endnotes
[1] National SCI Statistical Center, “Spinal Cord Injury (SCI) Facts and Figures at a Glance”, https://www.nscisc.uab.edu/Public/Facts%202016.pdf, accessed November 2017.
[2] Phillips, V. L, “Telehealth: Reaching Out to Newly Injured Spinal Cord Patients” in Public Health Reports 2001 Supplement 1, http://journals.sagepub.com/doi/pdf/10.1093/phr/116.S1.94, accessed November 2017.
[3] Agency for Healthcare Research and Quality, “Preventing Pressure Ulcers in Hospitals”, https://www.ahrq.gov/professionals/systems/hospital/pressureulcertoolkit/putool1.html, accessed November 2017.
[4] Shem, Kazuko and Sechrist, Samantha, “SCiPad: Effective Implementation of Telemedicine Using iPads with Individuals with Spinal Cord Injuries, a Case Series”, May 29, 2017, https://www.frontiersin.org/articles/10.3389/fmed.2017.00058/full, accessed November 2017.
[5] Beatty PW, Hagglund KJ, Neri MT, Dhont KR, Clark MJ, Hilston SA, “Access to health care services among people with chronic or disabling conditions: patterns and predictors”, Arch Phys Med Rehabil (2003), http://www.sciencedirect.com/science/article/pii/S0003999303002685, accessed November 2017.
[6] Smith MW, Hill ML, Hopkins KL, Kiralti BJ, Cronkite RC, “A modeled analysis of telehealth methods for treating pressure ulcers after spinal cord injury. Int J Telemed Appl (2012), https://www.hindawi.com/journals/ijta/2012/729492/, accessed November 2017.
[7] Zimmerman, Scott, “Insight: Tackling healthcare’s costly problem of missed appointments”, Healthcare Finance, April 24, 2015, http://www.healthcarefinancenews.com/blog/insight-tackling-healthcares-costly-problem-missed-appointments, accessed November 2017.



I really like the topic and the analysis you conducted, especially your point to evaluate these programs side by side using financial metrics. I think it would be interesting to see how telemedicine changes a doctor’s time allocation and productivity in correlation to the outcomes. Are patients better off because a doctor talked to them, or because there were specific things the doctor prescribed as a result of the “visit”? In other words, does telemedicine provide the placebo effect to patients? If so, can doctors reduce their overall time spent with patients, therefore, seeing more patients, and improving the supply chain and still maintain the same QoL for patients?
In general I have some doubts about patient willingness to adopt telemedicine because of the psychological barriers to sharing personal information with an unseen / unknown professional through a screen. What is interesting in this example however is that trust is already established through face to face time in the rehabilitation center, so I could see high value from introducing telemedicine to support long term condition management. Whether it really saves time in part depends on how effective remote diagnosis is (are the quality of images transmitted high enough, are doctors able to pick up on the subtle queues that prompt them to dig deeper etc). Only time and analysis of outcomes will provide the answer to this. It will also be fascinating to see how telemedicine fits into health insurance programs, which typically pay for activity. Should reimbursement tariffs for telemedicine be lower, and what incentives might this introduce?
As you discuss, it’s critical for the industry to consider both the impact on quality of life and cost to serve a single patient, as well as the total volume of patients served. Pending regulatory decisions on net neutrality may play a significant role in either holding back or promoting telemedicine. Current Federal Communications Commission rules make it illegal for internet-service providers (ISP) to block or slow content from a specific source. If the rules are repealed, ISPs may be able to charge more for telemedicine services because they tend to take up a lot more bandwidth than other sites. This would drive up internet costs and make telemedicine prohibitively expensive, especially for patients and hospitals in rural areas. Many questions are still up in the air – will net neutrality laws change? if they do change, how will ISPs react? even if costs increase for telemedicine, are the savings so substantial that it will just slow, rather than halt, adoption?
Alex, I thought your essay was well-researched, articulate, and well-defended. I am sufficiently convinced about the power of telemedicine, especially as it relates to the Santa Clara hospital system.
I would note, however, that telemedicine is not without its risks. Firstly, there are cybersecurity, privacy, and safety issues that need to be sufficiently addressed before telemedicine is rolled out more broadly. Secondly, is the hospital administration system open-minded? Oftentimes, they are the constituents who need to be convinced. The burden of proof is upon the technology provider to convince the hospital administration that it improves clinical outcomes (you provide compelling statistics above) while reducing costs. Thirdly, are physicians bought in? Would this reduce or diminish the role of person-to-person, mouth-to-mouth contact between physicians and patients? Finally, how do patients feel about this? Does this cheapen the medical experience?
Some of these risks are outlined in the article below. This is a compelling trend that will become the future. But when?
https://www.beckershospitalreview.com/healthcare-information-technology/overcoming-4-challenges-in-implementing-telemedicine-healthcares-next-frontier.html
Thanks for writing about this topic. This is very interesting and not discussed enough. I strongly believe that tele-medicine is an unstoppable reality. In Brazil, my home country, conservationism and strong regulations have, unfortunately, not allowed for tele-medicine to start and gain momentum as it is happening in other parts of the world, including the U.S.. A point that often comes up when discussing disruptive advancements in healthcare is what is the best for an individual patient VS what is the best for the society and the combination of all the patients. This point is so controversial because, we all think about ourselves or someone that we love in need of a specific healthcare treatment, and we always think that this person deserves what is the best possible out there. However, because resources are limited the best possible for each individual patient might not correspond to what is best for society. In my opinion, tele-medicine and the work that SCVMC is doing is one those cases. We still have a long way before we can say that a remote visit from a CSI specialist will be as good or effective as physical visit of the same specialist. Yet, it will be easy to prove that using this remote/virtual approach will yield better results for all the patients of the system. Therefore, I do not think we should ask “how will SCVMC ensure that these consultations achieve parity in quality?”, because these modes will hardly have the same outcome, (although this should be pursued as a vision). Instead, we should ask ourselves how can we prove that the tele-medicine will improve healthcare access and quality for the society as a whole.
Should this program be widely available for all patients, or those that have exceptional difficulties reaching the hospital?
My initial thought after reading this question that you posed was about pricing. Are telemedicine providers pricing these telemedicine visits at a rate that reflects that while they can get the job done in certain instances, they are not the same as an in-person visit? Your essay mentions a lot about costs that would be saved within the healthcare system when implementing this more widely, but the price is a critical component in my eyes. Are the early adopters of telemedicine pricing these visits at a rate that is truly reflective of the scaled down resources they need to conduct a telemedicine appointment? I am not insinuating price gouging, but there are probably many ways to arrive at the appropriate way to price a virtual doctor’s visit. What are health insurance companies willing to cover for a virtual doctor’s office visit? If the quality really is high, as is suggested by the data in this article, there should not be a difference. But perception is reality, and I imagine the perception of a virtual doctor’s office visit will mean that insurers will need to see a lot more data before there is a widespread determination about how similar prices for this offering should be to “normal” visits. Given this, I think keeping this limited to people in rural areas is best, so that they quality argument for this can be built up before it is rolled out across all consumers.