Re-inventing the medical device supply chain: How is Philips leveraging digitalization to up the ante?

Supply chain advances, through predictive analytics and remote upgrades in medical devices, are enabling the transition to value-based care.
Digitalization has emerged as a new area of interest in supply chain for medical device companies. On the one hand, it poses a threat from established technology companies expanding into healthcare. On the other hand, it provides opportunities for medical device companies to provide cutting-edge services to hospitals, improve their partnerships with healthcare providers, and enable the transition towards value-based care.
Why does digitalization matter?
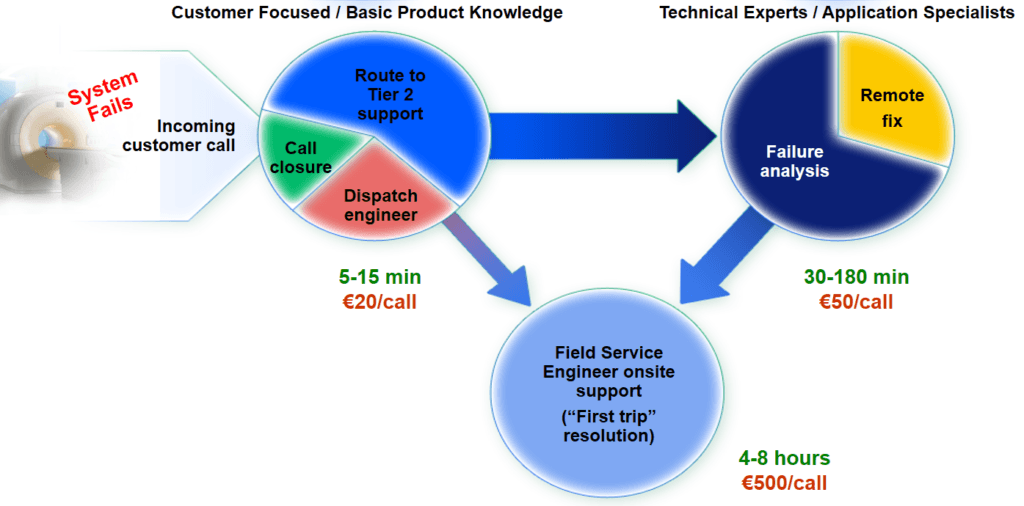
Medical device companies have traditionally relied on the reactive service model for post-sales maintenance and repair. The process begins with an incoming customer call from a hospital department. A vast majority of these calls would be routed to technical experts. About half of these calls would result into onsite support by an engineer. This reactive approach often leads to poor system availability, diminished performance of healthcare assets, and a substandard workflow. The entire process is slow and expensive for both the provider as well as the medical device manufacturer. In addition, it leads to a high down time of ~1%.
How is Philips leading the way?
Connected devices (internet of things), big data, and predictive analytics have provided unforeseen solutions to the problems in maintenance and repair of medical devices. Philips, one of the major players in medical device equipment, has leveraged these trends to offer cutting-edge supply chain solutions – remote upgrade and predictive maintenance. Philips can now remotely identify imaging system errors, diagnose the cause, and finally, troubleshoot and implement repairs. All of this has helped reduce the downtime to 0.1% in several partner hospitals.
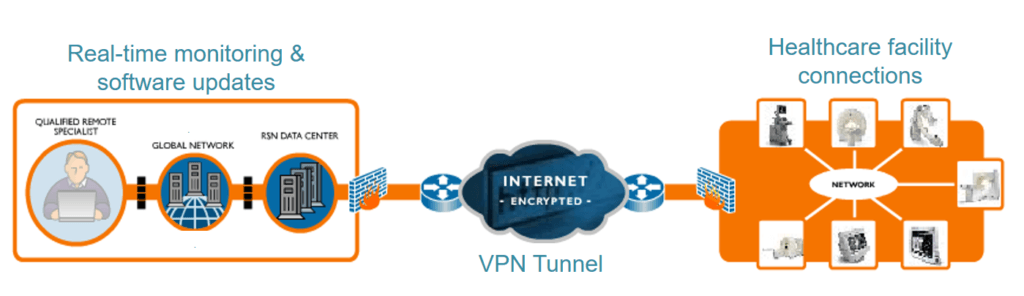
Remote upgrade has been a constant feature in smartphones, but was only recently picked up by medical device companies. Philips, in turn, has started upgrading its new diagnostic machines remotely, just as Apple would do for your iPhone. The product team schedules and pushes software updates automatically, and maintains software revision records through ERP system integration. This minimizes system downtime since updates can be performed off hours, maintains latest system software revisions for increased performance, compliance, and security, and reduces travel and workload for internal field engineers.
Predictive maintenance refers to service events being triggered by careful analysis of system data through data analytics algorithms and, therefore, before any major issues arise. These predictive alerts indicate that critical system and/or environmental parameters are out of specification. Philips diagnoses the problem remotely and, if possible, resolves the issue remotely. Otherwise a field service engineer is dispatched with guidance and needed parts for a single visit repair. This helps address system deviations proactively and preempt failures, avoiding system downtime, customer disruption, and associated costs. Further, it improves workforce and spare parts planning, and allows for continuity of care.
In the long term, Philips is looking to re-invent the medical device supply chain by shifting to diagnostics-as-a-service rather than as-a-product. Recently, it launched a portable ultrasound that connects to a tablet, providing incredibly low costs and sharing capabilities. It further began piloting a fee-for-service model for this device based on the number of tests conducted. While it enables the hospital by lowering capital costs, and by increasing accountability for value-based care, it provides opportunities for Philips to continuously engage with the providers, and provide value-added services. However, scaling the new model requires significant upskilling of sales and supply management capabilities. It would also be a challenge to build such products for other bulky diagnostic service machines, such as CT scan, MRI, and X-ray.
What more can Philips do?
Building on their success, Philips can leverage two other opportunities. First, engage in risk-sharing deals with hospitals. Philips can use the data that is now available from its devices, develop a better understanding of the risk of the population, and offer diagnostic services as part of a risk-sharing deal. Second, integrate diagnostics into a broader population health proposition. This could either be a part of bundled payments, or capitation payments model.
However, further progress in use of healthcare data is dependent on Washington D.C.’s ability to shift the patient data ownership to patients from providers. Lack of patient data continuity is a major roadblock for companies, such as Philips, that are looking to broaden the horizons of digital health.
Open questions:
1. What control mechanisms should a medical device company put in place so that a high pace of innovation does not create additional regulatory risks?
2. What are the various business models to offer diagnostics-as-a-service rather than as-a-product? Are there any parallels in another industry where Philips can find inspiration for such a model?
3. How can private enterprises play a stronger role in advocating patient data ownership?
(Word count: 781)
References
“Art & Science Of Service – Bentley College”. 2017. Atc3.Bentley.Edu. http://atc3.bentley.edu/conferences/service09/.
“Customer Services Solutions | Philips Healthcare”. 2017. Philips. https://www.usa.philips.com/healthcare/resources/landing/aiming-for-zero.
“Enjoy ‘Peace Of Mind’ With Remote Services”. 2017. Incenter.Medical.Philips.Com. http://incenter.medical.philips.com/doclib/enc/fetch/2000/…vernum%3d-2.
“Philips Lumify | Portable Ultrasound Machine”. 2017. Lumify.Philips.Com. https://www.lumify.philips.com/web/.
Sipos, Ruben, Dmitriy Fradkin, Fabian Moerchen, and Zhuang Wang. 2014. “Log-Based Predictive Maintenance”. Proceedings Of The 20Th ACM SIGKDD International Conference On Knowledge Discovery And Data Mining – KDD ’14. doi:10.1145/2623330.2623340.
“Two Different Maintenance Strategies In The Hospital Environment: Preventive Maintenance For Older Technology Devices And Predictive Maintenance For Newer High-Tech Devices : Table 4”. 2017. Hindawi.Com. https://www.hindawi.com/journals/jhe/2016/7267983/tab4/.



Thank you, Sushant! I found this essay very interesting, especially with your insight as an ex-Philips employee. Digitalization is a super trending topic in medical device industry currently, and as you pointed out, the focus of such digitalization is really the shift from “diagnostics-as-a-product” to “diagnostics-as-a-service”. I personally think what Philips has done so far in terms of remote upgrade and predictive maintenance makes a lot of sense from the cost and efficiency perspective, however, do you have any report or data showing the acceptance of physicians and patients? For instance, will patients push back because they don’t feel 100% safe to take a CT scan right after the system upgrade? In addition, the ownership and use of patients data is probably a more controversial topic. Will hospitals and patients be willing to share their data with the medical device providers, or the data should be provided on an as-needed basis?
Sushan this is a great essay! I agree with that predictive maintenance and remote upgrades will significantly increase machine utilization and allow manufacturers to gather data on device performance, usage etc. On the other I also agree with Bill on that remote services raise a question about the reliability from patients’ perspective. If I were a patient I would be reluctant to get a scan in a device right after the upgrade or remote maintenance service. I think Philips should start an initiative to educate patients and get their approval about its innovative services both to decrease regulatory risks and also use patient data to further innovate the industry. Moreover, Philips should introduce a comprehensive set of control mechanisms to avoid any failures because the damage caused by a software upgrade might cost a person’s life. To give an example, Philips can get in contact with device operators in hospitals and ask them to make several test runs before they start scanning patients. Creating a two-factor authentication process before starting daily operations will decrease risk of causing any irreversible damages. I believe this is only one aspect of the challenges and if Philips is going to innovate the industry they should invest in control mechanisms as much as new technologies.
Sushant, thanks for sharing your insight on the great work being done at Phillips to leverage digitalization to improve the medical device supply chain. From the maintenance standpoint, it sounds like the major shift is from a reactive to a proactive approach. The 90% reduction in downtime from this proactive approach is considerable. While average MRI charges vary between hospitals, sources suggest that the average cost is approximately $2-3K per scan (http://time.com/money/2993644/why-health-care-costs-vary-widely/). How is Philips pricing the value of the increased revenues for providers from this proactive approach into the service cost? Will providers or administrators be charged on a fee-per-upgrade or fee-per-service basis or does Philips plan to bundle this under a one-time maintenance fee at the point of sale? From a quality perspective, will providers be notified of the content of the remote upgrades in advance and is there an option for providers to reject an upgrade before it is made? While I think these innovations are great, the cost and quality implications must be addressed before I see this being widely accepted in hospitals.
This is great, Sushant! One big issue this raises in my mind around patient ownership of data is the need for a company like Philips to build trust with patients. As others here have mentioned, there may be some concerns about patients getting a scan right after an upgrade, etc. Beyond that, though, if Philips were to advocate for patient ownership of data, they’d need to be sure that patients would entrust them with that data. When it comes to someone as sensitive as medical care and health issues, that could be a hard sell. So, how can Philips be extra cautious with data to avoid bad PR and be sure that patients would be open to these agreements.
Another questions this raises for me around the idea of remote upgrades, etc. is how comfortable the healthcare providers (nurses, physicians, etc.) would be performing a scan or other service right after an upgrade. How confident is Philips with their upgrades? I know, for example, sometimes an iPhone upgrade can mess up or slow down other important parts of my phone and then Apple will quickly release another patch. In the medical field, this kind of difficulty is harder for people to overlook. So, what is the pace of upgrades from Philips and how much are they tested before being rolled out? Then, again, if the process is seamless, are the people using the equipment both prepared to use it and comfortable using it knowing about the upgrades, etc. happening behind the scenes? I think this needs to be addressed before I see Philips having broad success with some of these initiatives, although I agree they are innovative and necessary.
Thanks Suchant for sharing. Really interesting to read an article where the author has more experience than researching this for a few hours (I wish I could say the same about my paper). The remote upgrades make a lot of sense and decreasing downtime by 90% sounds awesome. But is there more that digitization can do to decrease the costs of scans like a CT scan?
Going from 1.0% to 0.1% is less than a 1% increase in # of scans that can be performed right? That doesn’t seem to drive down the per use cost much or increase access. Is there ways digitization could make shared use of resources more practical for a group of hospitals? For things like CT scan could digitization help coordinate scheduling to increase utilization of scanning machines to closer to 100%. What if in Boston for example there was one centrally located hospital that had more CT scan machines and ran CT scans 24/7 for that hospital + people who are well enough to travel. You could imagine that for more price-sensitive customers, they could choose to do a middle of the night or weekend scan and pay less. Whether this makes sense assumes a lot of the cost of a scan is fixed and not variable, and maybe things like this make no sense. But I’m hopeful that digitization can help address some of the explosion of costs in the medical field by decreasing the cost of scans.
Great analysis Sushant! Definitely interesting to read about the remote upgrade and predictive maintenance movement by Phillips, especially in an industry where digital innovations can often be excruciatingly slow.
I also think Phillips’ strategy to market it’s new ultrasound technology as a diagnostics-as-a-service model is smart. However, I wonder if this would further perpetuate the high healthcare costs we are seeing today, caused in large part due to the fee-for-service model as opposed to value-based healthcare. With such expensive technologies, I can see how it might make sense for the hospital to not capitally invest in the device itself. However, I can also see a problem in which companies like Phillips are incentivized to push this treatment in all cases, even when it does not add value, thus improving their revenues but putting a cost burden on the payers even when value is not added.
This is an innovative use of digitization to implement predictive maintenance on the medical devices. I can think of a parallel to this approach as we were using a similar technique to monitor the condition of the railway assets to leverage the power of predictive maintenance.
When digitization is applied to medicine and held by 3rd parties an important concept of personal information and security starts emerging. I believe the fields of cyber security will also develop in synchrony to protect the valuable yet personal data that these devices capture.
Additionally, as the medical devices start churning data for analysis, useful insights can be developed not just to advance the field of medicine but also related industries such as insurance will progress.
As information becomes paramount, various industries will move towards value based services, evolving the business models away from the assets and devices that serve them.
Thanks for this brilliant read, Sushant. Found it to be very informative.
I am a big fan of diagnostics-as-a-service model. While it helps traditional hospitals lower costs, I think the biggest value proposition is in the data that Phillips is able to aggregate and what they do with that data. Legalese aside, this model could bring access to rural areas and under-served populations who would likely be willing to share their medical data in exchange for such valuable access to diagnostic products.