Memorial Sloan Kettering Cancer Center: Leveraging Technology To Improve Cancer Treatment

Digital transformation creates huge opportunities for MSKCC and other hospitals to improve their quality of care and bottom line.
Memorial Sloan Kettering Cancer Center (MSKCC) is the world’s oldest and largest private cancer center, with a business model centered around providing high quality healthcare to patients.[1][2] MSKCC has embraced digitization to benefit patients, physicians, and the entire organization as seen through their adoption of electronic health records, and collaborations with Flatiron Health and IBM. Digital technology allows MSKCC to improve their operating model, providing high quality care in a quicker and smoother fashion, and expand their business model, finding new ways to create and capture value.
Electronic Health Records
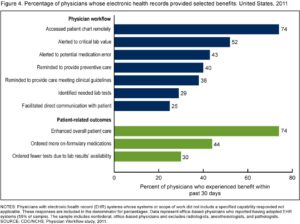
Electronic health records (EHRs) leverage digital technology to create a seamless flow of information at MSKCC, resulting in benefits ranging from improved patient safety and satisfaction to improved physician efficiency and accuracy.[3][4] EHRs are digital versions of paper charts, containing a patient’s full medical history from all providers.[5] EHRs provide physicians with more complete information about the patient, improving their ability to make well-informed treatment decisions.[6] EHRs also alert physicians to potential medication errors and remind them to meet clinical guidelines.[7] The resulting improved care and reduced errors make it easier operationally for the hospital to deliver on their customer promise. Further, productivity gains allow for a faster delivery of that quality care.[8]
EHRs offer MSKCC important financial benefits relative to hospitals not leveraging this technology. Faster charge capture and fewer billing errors drive improved cash flow and revenue.[10] The electronic availability of information also reduces costs, eliminating unnecessary tests and the costs of maintaining paper files.[11] EHR adoption however has some drawbacks: high acquisition costs, ongoing maintenance costs, and privacy concerns.[12]
Flatiron Health Collaboration
MSKCC, embracing the digital revolution, recently partnered with Flatiron Health.[13] Flatiron is using technology to solve the problem of lost and unleveraged data on oncology patient treatment journeys. Flatiron’s goal is to collect patient outcomes data on a common searchable platform to improve cancer care.[14] MSKCC, by partnering with Flatiron, will be contributing to the database development, and benefiting from the collective learnings from cancer patients across the country through access to an aggregated outcomes database.[15] This partnership enables efficiencies in delivering quality healthcare and patient satisfaction. The ability to better anticipate the right drug for a patient, leveraging insights from similar patients’ outcomes beyond their own center’s walls, helps even the best physicians optimize results. Further, sharing insights with oncology providers broadly through the Flatiron platform expands our perception of the value a hospital can provide – beyond just providing quality care in their own hospital, to providing this value more broadly across the country.
IBM Watson Collaboration
IBM Watson is a supercomputer that can function as a doctor running through thousands of clinical studies, patient records, and medical textbooks to deliver a diagnosis and treatment plan.[16] MSKCC partnered with IBM to develop the “Watson for Oncology” application, training Watson to think like MSKCC experts in oncology, so doctors anywhere can access this level of expertise through licensing the program.[17] With this partnership, MSKCC is showing they don’t want to just use technology to better their own operations, but they want to be involved in the democratization of information, leveraging technology to better cancer treatment worldwide. For this contribution, MSKCC had a shared revenue agreement with IBM, contributing to the changing business model for the hospital.[18] With this partnership MSKCC is further expanding the scope of its business model and value proposition beyond providing quality outcomes for their own patients to impacting the treatment of patients worldwide. Before this partnership, MSKCC was impacting broader cancer treatment through clinical trials and research publications, but with this technology they can dispense information in a more usable format, to the point that within seconds a patient in India can have a diagnosis and treatment plans specific to their needs.[19]
Additional Steps
MSKCC’s use of EHRs and collaborations only provide a glimpse into how healthcare and technology are partnering to create and share value. Robots are already being used in hospitals to deliver drugs and clean up medical waste, letting humans take on more complex tasks and cutting costs.[21][22] MSKCC could benefit from adopting robots to fill these and other roles. Remote monitoring programs, alerting physicians to vitals and other biometric data requiring careful watch after patient discharge, allow for cost savings in readmissions.[23] MSKCC could use these programs to monitor high-risk patients after chemotherapy or outpatient transplants.[24]
MSKCC leverages digital technology to improve their value proposition of providing quality healthcare, the way they go about delivering that care, and their bottom line. Though navigating the expanding amount of data available today can be challenging for hospitals, MSKCC demonstrates how to chart the path forward to their benefit, placing themselves in a key position in big data initiatives by fueling the learnings of databases and machines, and adjusting their business model to capture value around these new opportunities.
Word Count: 800
[1] Memorial Sloan Kettering Cancer Center, “About,” https://www.mskcc.org/about, accessed November 2016.
[2] Kenneth Kaufman, “The Five Key Elements to a Hospital’s Value Proposition,” Hospitals & Health Networks, October 22, 2015, http://www.hhnmag.com/articles/6641-the-five-key-elements-to-a-hospitals-value-proposition, accessed November 2016.
[3] “Leading cancer center selects Allscripts dbMotion™ and renews Allscripts Sunrise™ relationship to facilitate exceptional community-based patient care,” press release, July 9, 2014, on Allscripts website, http://investor.allscripts.com/phoenix.zhtml?c=112727&p=RssLanding&cat=news&id=1945965, accessed November 2016.
[4] “How Electronic Medical Records Reduce Costs and Improve Patient Outcomes,” Smart Business LA County, July 12, 2010, https://www.memorialcare.org/about/pressroom/media/how-electronic-medical-records-reduce-costs-and-improve-patient-outcomes-2010, accessed November 2016.
[5] “What Is an Electronic Medical Record (EMR)?” HealthIT.gov, https://www.healthit.gov/providers-professionals/electronic-medical-records-emr, accessed November 2016.
[6] Ibid.
[7] “Benefits of Electronic Health Records (EHRs),” HealthIT.gov, https://www.healthit.gov/providers-professionals/benefits-electronic-health-records-ehrs#footnote-1, accessed November 2016.
[8] “How Electronic Medical Records Reduce Costs and Improve Patient Outcomes,” Smart Business LA County, July 12, 2010, https://www.memorialcare.org/about/pressroom/media/how-electronic-medical-records-reduce-costs-and-improve-patient-outcomes-2010, accessed November 2016.
[9] Eric Jamoom, Paul Beatty, Anita Bercovitz, et al., Physician Adoption of Electronic Health Record Systems: United States, 2011,” National Center for Health Statistics, July 2012, http://www.cdc.gov/nchs/products/databriefs/db98.htm, accessed November 2016.
[10]Nir Menachemi and Taleah Collum, “Benefits and drawbacks of electronic health record systems,” Risk Management and Healthcare Policy 4 (2011): 47-55, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3270933/, accessed November 2016.
[11] “Medical Practice Efficiencies & Cost Savings,” HealthIT.gov, https://www.healthit.gov/providers-professionals/medical-practice-efficiencies-cost-savings, accessed November 2016.
[12] Nir Menachemi and Taleah Collum, “Benefits and drawbacks of electronic health record systems,” Risk Management and Healthcare Policy 4 (2011): 47-55, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3270933/, accessed November 2016.
[13] Matthew Tontonoz, “Between the Moon and New York City: Vice President Biden Leads MSK Cancer Moonshot Roundtable,” Memorial Sloan Kettering Cancer Center Blog, May 27, 2016, https://www.mskcc.org/blog/between-moon-and-new-york-city-vice-president-biden-leads-msk-cancer-moonshot-roundtable, accessed November 2016.
[14]Flatiron Health, https://flatiron.com/, accessed November 2016.
[15] Matthew Tontonoz, “Between the Moon and New York City: Vice President Biden Leads MSK Cancer Moonshot Roundtable,” Memorial Sloan Kettering Cancer Center Blog, May 27, 2016, https://www.mskcc.org/blog/between-moon-and-new-york-city-vice-president-biden-leads-msk-cancer-moonshot-roundtable, accessed November 2016.
[16]Laura Lorenzetti, “Here’s How IBM Watson Health Is Transforming The Health Care Industry,” Fortune, April 5, 2016, http://fortune.com/ibm-watson-health-business-strategy/, accessed November 2016.
[17] Ibid.
[18] Ibid.
[19] Peerzada Abrar, “IBM’s Supercomputer helps doctors to fight cancer,” The Hindu, August 7, 2016, http://www.thehindu.com/business/ibms-watson-helps-doctors-to-fight-cancer/article8955898.ece, accessed November 2016.
[20] Bloomberg, “IBM’s Breakthrough: Watson May Help Beat Cancer,” YouTube, published May 23, 2013, https://www.youtube.com/watch?v=HkEOJnn_zlg, accessed November 2016.
[21] Matt Simon, “This Incredible Hospital Robot Is Saving Lives. Also, I Hate It,” Wired, February 10, 2015, https://www.wired.com/2015/02/incredible-hospital-robot-saving-lives-also-hate/, accessed November 2016.
[22] Ross Crawford, Anjali Jaiprakash, and Jonathan Roberts, “Robots in Health Care Could Lead to a Doctorless Hospital,” SingularityHub, February 10, 2016, http://singularityhub.com/2016/02/10/robots-in-health-care-could-lead-to-a-doctorless-hospital/, accessed November 2016.
[23] Lola Butcher, Paul Barr, and Suzanna Hoppszallern, “2016 MOST WIRED,” Hospitals & Health Networks 90 (2016): 30-43, http://search.proquest.com.ezp-prod1.hul.harvard.edu/abicomplete/docview/1807005237/in real time913D3F72EF4845F0PQ/13?accountid=11311, accessed November 2016.
[24]Michael Thompson, “Does Telemonitoring Have a Place in Oncology?” ASCO Connection Blog, May 3, 2012, https://connection.asco.org/blogs/does-telemonitoring-have-place-oncology, accessed November 2016.



Really interesting and inspiring post. It is great to see a large, private institution trying to democratize data to help people all over the world. I am a firm believer that data needs to become a bigger part of patient diagnosis and management. Many physicians do not stay up to date on the latest medical treatments and PCPs in rural areas are unlikely to have experience with rarer forms of diseases. Having Watson have an 85-95% accuracy and being used in conjunction with doctors could really save lives, provide earlier diagnoses, and help identify the most effective treatments.
Thanks for sharing this post. It’s incredibly cool to see what MSKCC is doing in the digital space. I’m also glad you touched on the cost aspect of building EMRs because I think that’s going to be an important consideration in determining the future of health care in the US. Large providers require huge, complex systems to manage their care, even at specialty hospitals like MSKCC that provide a limited set of services. This often requires millions of dollars in external consultant fees both upfront and every time there’s a system upgrade or problem. MSKCC is one of the most respected hospitals in the world and as such is able to take in a ton of resources. Many community hospitals and smaller providers are getting left behind in the digital revolution because they can’t afford the high price of a lot of these innovations.
It is great that Memorial Sloan Kettering is striving to make better use of its data to improve quality and efficiency of care. With all of these initiatives, I wonder what mechanisms it has in place to warehouse its data. With provider consolidation continuing to occur, providers within one overall system will often have multiple different EHR systems in place across the multiple inpatient and outpatient settings that comprise the integrated system. Furthermore, EHRs are just one of multiple data sources that are relevant to providers as they work to improve quality and efficiency of clinical care. To add to the problem, once health systems have implemented an EHR, they must organize, visualize and utilize this data through a healthcare-ready data warehouse infrastructure to identify and act upon the data. As long as healthcare data sits in the various clinical and operational systems (silos), it is not available for analytics.
One company tackling this fundamental problem in data warehousing is Salt Lake City-based Health Catalyst, which has taken a leadership position in the enterprise data warehousing (EDW) market. In the last year, the company announced a 10-year, $100mm agreement with Allina Health as well as long-term relationships with UPMC, Cedars Sinai and Partners Healthcare. I would be curious to understand how Memorial Sloan is tackling this problem.