Iora Health: Improving Health While Cutting Costs
Mission and Business Model
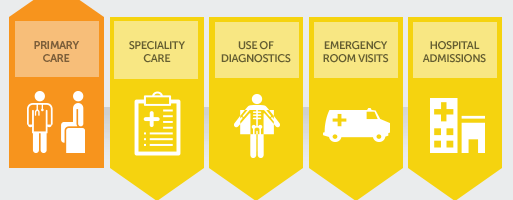
Iora is a for-profit primary care model that aims to create value by improving patient health while lowering overall cost to the patients’ employers. Their business model is to provide high quality and service-oriented primary care to help patients better manage their health, keep them out of emergency rooms and hospitals, and drive down overall per patient health care costs.
Their target customers are unions and large employers who pay a flat monthly rate of $50-60 per patient for primary care services through Iora for eligible employees.3 This amount is double what these employers are used to paying for primary care.4 However, Iora advocates that this investment in preventive and patient-centered care can actually decrease cost drivers like patient hospital visits, which averages about $10,000.00 per stay.5
Key Elements of Operating Model and Model Alignment
–Aligning financial incentives with mission: Much of health care still operates under a fee-for-service model where providers are compensated for specific tests or procedures they run. This kind of compensation encourages high-volume and the overuse of unnecessary tests. In order to better align cost saving, patient satisfaction, and improved health, Iora adopted a flat monthly fee per patient. Thus, providers were incentivized to maintain costs under this amount while also providing good patient service with quality care in order to retain patients as customers. This payment model also has the added perk of cutting out expenses related to billing paperwork.2 By moving away from a fee-for-service model, doctors have more time to spend with their patients, which leads to happier and healthier patients.6 Additionally, Iora was able to develop systems to cater to patients needs, such as a same-day scheduling system for acutely sick patients and extended availability of staff for patient inquiries. 2 All in all this easy and convenient access to care that made patients feel respected and cared for led to increased primary care follow-ups and lower usage of emergency room and hospital visits.1

–Strategic labor decisions: One key aspect of Iora’s operating model is the team-based approach to care. Some of the most vital members of the team are “health coaches” who see patients even more frequently than doctors do for maintenance visits, and update physicians about the patient’s progress. They are hired for their communication abilities, and the biggest value-add is their ability to connect well with patients and serve as their advocates.2 They work with patients to set up referrals, work through strategies for medication adherence, and may even accompany patients to the grocery store. Iora’s team-based approach also promotes the use of cheaper labor—such as behavior health specialists, nurses, and health coaches—when possible, which allows doctors to only be utilized for services they are uniquely qualified to provide, which in turn drives down labor costs.2
–Use of analytics to measure and ensure quality: Iora has prioritized finding ways to collect data in order to help improve their processes. For example, patients send in routine measurements of blood pressure and glucose that are taken at home and providers can monitor these numbers remotely and make treatment changes as necessary. Additionally, health coaches are notified if patients do not pick up medications, and they can follow-up with these patients to encourage medication adherence. These checks help Iora identify potential issues early on so that patients can stay out of the hospital.
Overview of the Iora Model in the words of patients and provider team members:
Iora as an Example of Effectiveness
I chose this company as an example of effectiveness because they have pioneered a method of delivering primary care that preliminary studies have shown is fulfilling their goals. There was “an average 48 percent drop in emergency room visits and a net spending reduction of 12.6 percent [for their patients] in Atlantic City and 20 percent in Seattle” in a study conducted a year after implementation.4
Possible Challenges:
This model is a compelling one, but some questions remain about future potential and continued alignment of business and operational models. For one, it will be important to follow patients long term to ensure that the improved health outcomes and decreased health resource usage mentioned above is a sustained finding over the course of the patients’ lives. Additionally, there is the question of scalability in the current health care context. While health care is slowly moving towards more value-based payment models, like the one described above, most providers and payors still focus on a fee-for-service based approach. Even now, Iora is sometimes asked to file “dummy claims” because they are caught in the middle of this transition. Operating as both a fee-for-service and as a value-based service does not allow for aligned business and operational models and leads to additional costs.8 Furthermore, Iora works because they are getting large employers to sign employees up for their services, but what will it take for large governmental insurers like Medicaid and Medicare to change practices from fee-for-service to value-based payments? And as this health care delivery system becomes more popular, how will the operational model adapt to an influx of patients?
All Images from: http://www.iorahealth.com/real-results/
- http://www.iorahealth.com/real-results/
- http://www.newyorker.com/magazine/2011/01/24/the-hot-spotters
- https://www.bostonglobe.com/business/2015/05/03/iora-health-pioneers-new-primary-care-model/kc7V4W5V8OJ0gxFqY4zBrK/story.html
- http://www.bizjournals.com/boston/blog/startups/2012/08/iora-health-boston-primary-care.html?page=all
- http://www.beckershospitalreview.com/finance/11-statistics-on-average-hospital-costs-per-stay.html
- http://www.wsj.com/articles/the-u-s-s-ailing-medical-system-a-doctors-perspective-1409325361
- https://vimeo.com/134095032
- http://healthaffairs.org/blog/2015/08/17/breaking-the-fee-for-service-addiction-lets-move-to-a-comprehensive-primary-care-payment-model/



While they seem to provide an effective preventative care model, their business model would worry me in their ability to adequately create value that their business clients can actually see. Since they only perform ambulatory care, the businesses need to purchase additional health insurance for any inpatient care that’s still needed. So while they may create cost savings, they still require the client to carry all of the risks. What makes them preferable to more comprehensive preventative care coverage (like an HMO)? I would be curious to know if they have looked at partnering with hospitals and expanding their value proposition to cover both inpatient and ambulatory services.
Interesting piece, Iora has received lots of attention in health care, and for good reason. One question I have though, you often hear about new models like Iora being better because they allow for same-day scheduling and other similar fast services; what in the Iora model allows such quick patient responsiveness to occur that doesn’t happen in other PCP settings? Is it that physicians have more scheduled down-time during the day when they aren’t seeing patients? If so, some may argue that that’s not efficient use of the physician’s time. Where is the flexibility in scheduling and provider resources built in to see patients on a same-day basis? Also, interesting that the value-based-payment model works as well here as it does given that PCPs won’t necessarily see the increased costs of an admission to a hospital (unless their already in an ACO-type model).