A Hospital’s $1.2 billion Digital Transformation

“this is not an IT implementation, this is a business transformation”
In 2009, President Obama signed into law the Health Information Technology for Economic and Clinical Health Act (HITECH Act) as part of an economic stimulus package. HITECH’s primary goal was to increase the number of healthcare providers using electronic health records (EHR) as opposed to paper ones. Starting in 2011, healthcare providers that could prove “meaningful use” of EHR software would receive substantial government subsidies [1]. In 2015, the economic incentive would flip to an economic penalty and providers not using EHR’s would lose out on a percentage of government Medicare and Medicaid reimbursement [2]. Although the deadline was subsequently pushed back due to slower progress than expected, the legislation has been successful in catalyzing a trend towards the digitalization of healthcare. EHR adoption is clearly the way of the future and is no longer a question of if but when.
Partners Healthcare, a large Boston-based hospital system, is in the midst of its multi-year and $1.2 billion EHR implementation [3]. According to Keith Jennings, the Chief Information Officer at one of Partners’ affiliate hospitals, “a project like this, this is not an IT implementation, this is a business transformation for your clinical systems, your clinical user” [4]. The business model transformation Jennings mentions has to do with how EHR’s change the entire healthcare delivery system.
EHR’s improve healthcare quality by increasing coordination across all of the settings that a particular patient receives care. Regardless of specialty or physical location, any doctor can immediately access a patient’s medical history. This information gives the doctor tremendous insight into the patient’s comorbidities, allergies, medications, and past treatments, which all factor into the doctor’s subsequent treatment plan. The software surrounding the EHR can also provide recommendations based on clinical guidelines and best practices for particular indications [5]. In addition to improved efficacy, EHR’s have the ability to save healthcare providers money through the elimination of duplicative tests, paper storage, etc. [6].
Despite its benefits, implementing an EHR system does not come without friction. The move from paper to electronic records has required a transformation in the way hospitals operate. Some healthcare providers find electronic data entry to be more efficient than paper methods, but others are overwhelmed by it. The Boston Globe cited sources who thought that the EHR brought an “insatiable demand for information that, keystroke by keystroke, click by click, overwhelms the already tightly wrapped day inside a hospital, eats away at time with patients, and sometimes forces them to work longer shifts” [7, 8]. It will likely take time and continuous training for Partners to unlock the bulk of the efficiencies offered by EHR. In order to ensure a smooth transition, Partners has hired hundreds of IT workers to prepare and optimize the software. It has also staggered the implementation in phases, so that learnings from one hospital can be incorporated into the next hospital’s implementation [7].
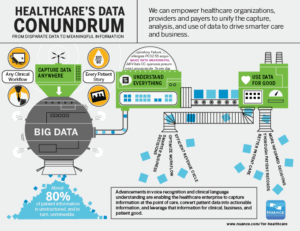
EHR implementation is just the tip of the iceberg for how information technology can revolutionize the practice of healthcare. As the number of electronic health records grows and time passes, the longitudinal health data they contain will be extremely valuable. It will allow for the comparison of treatment efficacy across patient types to help inform best practices and can also be used for predictive analytics [9]. Healthcare providers can use this data themselves or potentially monetize it through selling the data to pharma companies or software vendors. Despite all the current and future benefits, Partners Healthcare needs to be vigilant about the risks. EHR’s contain extremely sensitive health information, which means Partners must make sure it has a state of the art cyber security system that is continuously upgraded. Only time will tell the true costs and benefits associated with EHR implementation. (619 words)
Sources
[1] Search HealthIT, “HITECH Act (Health Information Technology for Economic and Clinical Health Act),” http://searchhealthit.techtarget.com/definition/HITECH-Act, accessed November 2016.
[2] National Business Coalition on Health, “Getting A Return on Electronic Health Record Investments,” http://www.nbch.org/nbch/files/ccLibraryFiles/Filename/000000003612/Getting%20A%20Return%20on%20Electronic%20Health%20Record%20Investments.pdf, accessed November 2016.
[3] Health IT & CIO Review, “8 Epic EHR implementations with the biggest price tags in 2015,” http://www.beckershospitalreview.com/healthcare-information-technology/8-epic-ehr-implementations-with-the-biggest-price-tags-in-2015.html, accessed November 2016.
[4] Search HealthIT, “Epic’s EHR: Challenges and lessons learned at Mass General,” http://searchhealthit.techtarget.com/video/Epics-EHR-Challenges-and-lessons-learned-at-Mass-General, accessed November 2016.
[5] Boston Globe, “Partners’ $1.2b patient data system seen as key to future,” https://www.bostonglobe.com/business/2015/05/31/partners-launches-billion-electronic-health-records-system/oo4nJJW2rQyfWUWQlvydkK/story.html, accessed November 2016.
[6] Health Affairs Blog, “A Standard Model For Evaluating Return On Investment From Electronic Health Record Implementation,” http://healthaffairs.org/blog/2014/01/06/a-standard-model-for-evaluating-return-on-investment-from-electronic-health-record-implementation/, accessed November 2016.
[7] Boston Globe, “New $1.2b Partners computer system brings prescription for frustration,” https://www.bostonglobe.com/business/2016/05/16/partners-healthcare-new-computer-challenges-some-doctors-nurses/1I4QsWGjCJ97xFmUbcDbaJ/story.html, accessed November 2016.
[8] McCullough, J. S., Casey, M., Moscovice, I., & Prasad, S. (2010). The effect of health information technology on quality in U.S. hospitals. Health Affairs, 29(4), 647-54. Retrieved from http://search.proquest.com.ezp-prod1.hul.harvard.edu/docview/204628452?accountid=11311)
[9] Electronic health records market (EHR) to grow at 5.53% CAGR to 2020 driven by digital and connected healthcare technologies. (2016, Jun 29). PR Newswire Retrieved from http://search.proquest.com.ezp-prod1.hul.harvard.edu/docview/1800114803?accountid=11311
Image Sources (in order of appearance)
Pulse Headlines, “Electronic health records are a major cause of doctors’ burnout,” http://www.pulseheadlines.com/electronic-health-records-major-doctors-burnout/37906/, accessed November 2016.
Partners Healthcare, “Partners HealthCare opens new Assembly Row complex, http://www.partners.org/Newsroom/Articles/Assembly-Row-Complex-Opens.aspx,” accessed November 2016.
HealthIT, “Predictive Analytics will Revolutionize Healthcare,” http://healthitmhealth.com/predictive-analytics-will-revolutionize-healthcare/, accessed November 2016.




What a fascinating read!
EHRs certainly are ushering in a new area for healthcare providers across the country. While the promise of EHRs are clear–providing all important medical information about a patient in a single, accessible place–I am concerned about 2 things: the cost of such systems and patient privacy. I understand that a lot of institutions are currently using Epic as their EHR. However, seeing that Partners spent over $1 billion to implement it at their site, I wonder how much further Epic can proliferate before other, lower-cost competitors (like the partnership between BIDMC and Athena Health) start to steal their market share. With that being said, does the promise of EHRs break down if different institutions are using different systems? A multitude of proprietary systems may not easily communicate with one another, keeping patient information as fractured as it is today. Secondly, I wonder if EHRs should be used as a database in which to analyze patient information in aggregate. Something feels “icky” to me about hospitals selling patient information (even if it is de-identified) to pharma companies or other research institutions. I wonder who should be seen as “owning” the medical information in EHRs–the hospitals or the patients? I personally think using the information for anything other than individual medical care brings up some troubling legal and ethical issues. It will be interesting to see how EHRs can deliver on their benefits while minimizing the potential complications in the future.
Thanks for the insightful read! I definitely see the role of EMRs in standardizing care in accordance with best practices/evidence-based medicine (through standardized workflows, medication reconciliation, etc.). One concern, which Mike brought up above, is interoperability. While many large health systems like Partners are deploying Epic, other hospitals–and independent physician practices–are deploying EMRs from a wide variety of other vendors. The fact that the systems do not seamless exchange data with one another negates many of the efficiency and patient safety (all records/immunizations/medications in one place) benefits of these systems. EMR providers are not presently incentivized to make their systems interoperable, so it will be interesting to see the development on legislation and other action to progress toward that goal.
Thanks for the great read! @Mike, @BJF – sounds like its time for us to start an interoperability company.
I hope that the EMR players can find a way to aggregate their data in a meaningful way. If we can put more sources together, data scientists will be able to draw connections between patterns of disease that can be used to help prevent illnesses instead of our current sick-care framework. Right now, insurance companies and life sciences companies are attempting to work through this, but no unified data source exists with information as rich as what is stored in EMRs. To Mike’s point, I do think individual patients should be the ones to consent to sharing data, even if it is de-identified. However, I think patients should also be educated on how this data can be used to improve medicine and bring better treatments faster.