Physician Engagement in this value Based Environment
Our hospital is a large University affiliated teaching hospital which is part of a larger network of hospitals.
In terms of quality, research shows that positive physician engagement benefits overall organizational performance. In our organization we have a high complacency rate with difficulty getting physicians to serve in a leadership capacity promoting and implementing changes in our healthcare delivery that create value and benefit for our patients.
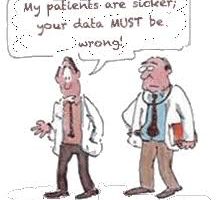
Many of the physicians find a thousand ingenious ways to withhold cooperation from a process that they feel is unnecessary. Even if the process is a regulatory requirement. It has become exponentially more challenging to get physicians sufficiently engaged to contribute to the greater benefit of the hospital system to improve quality and patient safety. some of the challenges include documentation requirements, following standardized protocols when indicated and communication with other team members to name a few.
We have a compensation model to reward physicians for good outcomes and use data analytics to monitor metrics and report outcomes. We also have multiple venues for physician recognition.
The current physician leader feels as though he is on an island and there is concern for rapid burnout
Clinical Problem:
1) How do you champion physician engagement to own clinical problems and be accountable for quality and patient safety.
2)Value based arrangements are a strategic priority. How do you align with the providers to share the risk.




Great question.
Although this conversation is about physicians, I believe the same can be said about most professions working in the healthcare industry.
A previous organisation that I worked for really excelled at team engagement. The following are noteworthy ways that engagement was fostered, perpetuated and maintained that may add to the ones you are already using to assist with Problem 1 and 2:
1. Use incentives that have meaning. As a rule, money incentives were never used, but incentives were matched with what that particular team/individual really valued. Most of the time, they did not have a significant cost profile, but they included a prime car parking space for a month, a voucher to their habitual lunch time restaurants (which means that they had to find out where you really liked to go), opportunity to present at a popular forum etc etc. The response to these incentives was powerful
2. Recruit with care. Some people are not suited to that balanced culture of innovation and accountability. If compliance is a real problem, then it would be discussed in interviews, at the time of sign on and then again at orientation. People were let go in their probation period if they exhibited behaviours of ‘not-caring’. This was tough for the team in the short-term as it increased everyone’s clinical load, but beneficial in the long-run.
3. Rigorous non-negotiable maintenance: Standards were set upon the commencement of employment and they were never allowed to slip. There was generally 1-2 people assigned to follow up and maintain a certain standard of care and they were particularly ‘tough’ on the leadership group to ensure that the correct example was set.
4. Celebrate and commiserate together. It sounds silly, but they really made simple efforts to support the team during great and not-so-great circumstances i.e flowers delivered to a doctors’ rooms when a loved ones dies, a bottle of wine with a card when they aced a conference presentation etc.
Sound easy…but as we know the reality is always more complex. But I still believe that unless the simple team engagement activities are performed, the larger change management will never occur.
Good luck!
Dear East Coat Connection,
To answer your first question, I may have to piss some of the physician in the group, so apology in advance.
1) How do you champion physician engagement to own clinical problems and be accountable for quality and patient safety.
Institution like hospitals cannot relay only on positive reinforcement. Once the benchmark for any Performance Indicator is set by the administration, all team player should abide by the roles and principles that govern this PI in order to achieve the minimum requirement or bench mark or national or interneuional average to be attained. So, physician should held accountable for sub optimal performance or not finishing their duties in timely manner such as filling their medical records by deadline then the chief of staff will issue a suspension memo for that particular doctor because also you do not to hold their colleagues accountable for their underperformance.
We had a surgeons had issues with hand sanitization before or sometimes after examining patients. First verbal warning did nit do any change believe or not, but when he get his first written warning after documentation by video tape that he did not wash his hands before entering patient room, the attitude changed 180 degree.
2)Value based arrangements are a strategic priority. How do you align with the providers to share the risk.
Like was mentioned before by, mission of your institution should be reinforced in orientation sessions (that you need to give it time f days like couple of days), during start of work (let HR be actively involved with new physician), then email and SMS reminders about key issues like hand sanitization, even let your team create Day for a problem you are struggling with and make it an event and ask all to participate like if you had a couple of insidence of HIPPA Violation, make HIPPA day.
Good luck