The Dr. Will See You Now…On the Screen
Despite being over 70 years old, Kaiser Permanente is leading the digital health transformation.
Healthcare costs have been on the rise and hundreds of digital health startups seeking a solution to lower costs. $3.9B was invested during the first half of 2016 in seed and Series A deals looking to shake up the heavily regulated and antiquated system.[i] Of that funding, there were a record-breaking 151 companies that raised more than $2M.[ii]
While there has been a huge influx of new companies into the healthcare space, Kaiser Permanente, one of the largest and oldest (since 1945) U.S. players has also been heavily investing in health tech and leading the charge on implementation.[iii]
Kaiser has had the same business model for years: they are both the insurer and provider, from primary care to hospitals. This model incentivizes them to lower the total cost of care and hence focus on preventative health and lower cost settings. Kaiser’s business model has been quite successful; in 2015, Kaiser generated about $60B[iv] in operating revenue while caring for 10.6M members.[v]
Despite their success, Kaiser is not resting on their laurels. Over the past several years, Kaiser has been upgrading their operating model, shifting to more technological solutions. Last year, Kaiser had more tele-visits than in-person encounters, 59M vs. 50M respectively.[vi]
While there are many telemedicine startups, Kaiser’s competitive advantage comes from their HMO model where members must see a Kaiser physician, resulting in the consolidation of their records in a single Electronic Medical Record. Kaiser patients receive (arguably) better care because those physicians have access to the patients’ complete record.
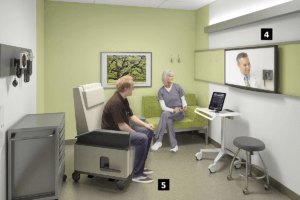
Kaiser recently opened several “health hubs” seeking to improve the experience of going to the doctor with online check in and co-pays, text alerts when the Dr. is ready.[vii] If a patient needs to see a specialist that isn’t at their site, they are able to do a video visit on the large screen in the exam room. These new exam rooms are expected to increase the number of visits by 20%-40% and to save 10% via space-conscious floor plans, and technologies and workflows.[viii]
Kaiser is also investing in longer term transformational research at their 37,000 square foot test warehouse in northern CA.[ix]
Some of the pilots include:
- Monitoring and tracking a patients’ living space for falls, sleep, diet, etc.
- Driverless car that can be dispatched out to the patient to determine if they need to go to the hospital.
While some ideas could seem far flung or questionable in efficacy, I applaud Kaiser for the focus on innovation and experimentation to question the status quo. Kaiser even started a venture capital arm to invest in digital health and quickly incorporate new technology.[x]
While Kaiser has had success in implementing and shifting toward digital solutions relatively quickly, it hasn’t been without issues. One IT upgrade cost $1 billion rather than the budgeted $500 million.[xi] Kaiser also faced some push back from the nurses in their Oakland hospital opening that

incorporated digital monitoring. The nurses were concerned about the reliability of the machines and some technicians were afraid of losing their jobs to these new machines. As a result, the local paper ran an article where some nurses claimed the heart monitoring machines had failed and the nurses had no way to know.[xii]
Kaiser should implement a change management program to help the techs, nurses, administrators, and physicians along the transformation journey as new technology impacts their role in delivering care. The negative reaction and press from the Oakland hospital could have significantly impacted the trust of the community. Some of the investments Kaiser is exploring could be incredibly beneficial and transformational changes for healthcare, but if they employees are not brought along and shown why they should trust the new way, Kaiser’s membership and employee morale could suffer.
(796 words)
[i] Susan Hall, “Health IT investments: Proven winners or scrappy startups,” Fierce Healthcare, November 16, 2016, http://www.fiercehealthcare.com/it/who-will-bring-health-it-transformation-and-how-soon?utm_medium=nl&utm_source=internal&mrkid=38888469&mkt_tok=eyJpIjoiWVRZME0yTmtObVJoTlRCbCIsInQiOiJ3ZDA2RFNcL2lLdXQ2VWRYUHRYSFpKN3FtejY4RlBIMW1jTHFsYnhiOFwvZyt6b0h1Zm1sdWJJdHNXcDV5bm40R05uc1wvdXhlNk9MSkM5dlUxVXhyWTl6YlJRQm1RdUdWaGFQNWZzMGVWcjBGaz0ifQ, accessed November 2016.
[ii] Mitchell Mom, Ashlee Adams, Digital Health Funding 2016 Midyear Review, Rock Health, https://rockhealth.com/reports/digital-health-funding-2016-midyear-review/, accessed November 2016.
[iii] “Kaiser Permanente’s ‘Health Hub’ Design Named a Finalist in Fast Company’s 2016 Innovation Awards,” Kaiser Permanente press release (Pasadena, CA, September 19, 2016) https://share.kaiserpermanente.org/article/kaiser-permanentes-health-hub-design-named-finalist-fast-companys-2016-innovation-awards/
[iv] Melanie Evans, Modern Healthcare, February 12, 2016, “Kaiser Permanente reports growth in membership, revenue in 2015” http://www.modernhealthcare.com/article/20160212/NEWS/160219960, accessed November 2016.
[v] Caroline Chen, “Taking Bids on the Hospital of the Future,” Bloomberg Businessweek, July 22, 2016, http://www.bloomberg.com/news/articles/2016-07-22/taking-bids-on-the-hospital-of-the-future, accessed November 2016.
[vi] Ibid.
[vii] Jeff Ferenc, “Kaiser Permanente opens first of community health hubs,” May 18, 2016, http://www.hfmmagazine.com/articles/2197-kaiser-permanente-opens-first-of-community-health-hubs, accessed November 2016.
[viii] Adam Bluestein, “Kaiser Permanente Designed a Health Center that Puts Patients First,” Fast Company, March 22, 2016, https://www.fastcoexist.com/3057404/world-changing-ideas/kaiser-permanente-designed-a-health-center-that-puts-patients-first, accessed November 2016.
[ix] Ibid.
[x] Robert Siegel, “What If Healthcare Could Start With Technology? — Bernard Tyson, CEO Kaiser Permanente”, The Industrialists Dilemma, February 12, 2016 https://medium.com/the-industrialist-s-dilemma/what-if-healthcare-could-start-with-technology-bernard-tyson-ceo-kaiser-permanente-5052658a6212#.2gm3yfyms, accessed November 2016.
[xi] Ibid.
[xii] Sam Levin, “The Trouble with Kaiser’s Technology,” East Bay Express, September 10, 2014, http://www.eastbayexpress.com/oakland/the-trouble-with-kaisers-technology/Content?oid=4067393



Thanks for sharing this post, Taylor! The topic of electronic medical records is near and dear to my heart, as I worked on an extensive deal back in my banking days for a company selling this exact service to hospitals.
While I agree that the benefits of adopting electronic records are enormous, I want to share some of the concerns I heard from hospitals when I was researching this topic. Other than the most prevalent concern of cost (hospitals were generally all pretty tight on budget and therefore unwilling to overhaul their existing systems), I encountered several doctors who complained about time constraints that electronic records placed on their jobs. Specifically, they said they had trouble demystifying the software and that took away time that they could have spent with additional patients. Hospitals were also concerned with the system’s vulnerability to crashes, which you can imagine could result in extreme consequences if the frequency or duration of incidence are high. My gut reaction to these concerns was to set up backup records systems, but we run into the same problem if the backup systems are also electronic. And if we created traditional paper backup systems instead, then doesn’t that defeat the purpose of implementing an electronic records system in the first place?
I think electronic medical records have made huge progress since I last visited the subject, but my main concern now is centralization. There are so many electronic record systems out there now and most of them are incompatible with each other, rendering the whole purpose of the system useless if patients were to switch hospitals. I am curious to see if there have been any major strides in this area of research.
[1] http://www.nytimes.com/2012/10/09/health/the-ups-and-downs-of-electronic-medical-records-the-digital-doctor.html
Taylor,
Thanks for bringing this issue up. While on the bleeding edge in terms of medical device technology and drug research, hospitals are notorious for their slow adoption of technology that administers the hospital.
You had mentioned telemedicine and I wanted to share one other area where telemedicine could potentially be very helpful. I think more than the example of Kaiser, which is obviously a highly scaled system with large provider locations near dense population centers, providers that are reaching those who live in rural areas are a better example of where telemedicine can be very helpful.
In the U.S., there is a troubling trend where doctors, and especially the best doctors, do not want to practice in the rural areas of the U.S. [1] Obviously, this would be a perfect area to use telemedicine, especially in areas such as therapy, where the physical proximity of the doctor is not as important. Luckily, studies have shown that video conference therapy is just as efficacious in treating mental diseases such as mood disorders, which affects 20-25% of all people in their lifetime [2].
All in all, I am excited to see what the future brings for medicine. I think we can all agree that there are many areas that are not only ripe for improvement, but must adapt in order to survive.
[1] August, 2014 The Atlantic “Why Are There So Few Doctors in Rural America?” Retrieved from http://www.theatlantic.com/health/archive/2014/08/why-wont-doctors-move-to-rural-america/379291/
[2] Stubbings DR, Rees CS, Roberts LD, Kane RT. Comparing In-Person to Videoconference-Based Cognitive Behavioral Therapy for Mood and Anxiety Disorders: Randomized Controlled Trial. Eysenbach G, ed. Journal of Medical Internet Research. 2013;15(11):e258. doi:10.2196/jmir.2564.
Thanks for the great post Taylor!
I find Kaiser fascinating for the reason you point out: they are both the insurer and provider. This allows them to align their incentives in a manner that many other networks can’t in order to generate the maximum value for their patients. I think telemedicine has a ton of potential and is largely underutilized because insurers are unsure of the potential results and in many scenarios unwilling to reimburse for it. Since Kaiser is the insurer, they have a lot more experimental flexibility and are taking a leading role in providing this service to patients. As you mentioned it can greatly reduced waiting time, improve space efficiency, and offers a great deal of convinience to patients. However, it certainly has limitations especially given the inability to perform a comprehensive physical examination. I am anticipating to see Kaiser have success in using this platform for a few specialties and expect them to encounter difficult with some of the more physical-exam dependent specialties. I’m also curious to see how they begin to use telemedicine on the inpatient setting to harness specialty expertise for difficult patients.
Thanks for the post, Taylor. KP’s payer/provider model is something that the rest of the healthcare industry should strive towards. I’ve done some work with them and find their ambition to be inspiring. For sure, they don’t plan to rest on their laurels, as you put it. Telemedicine is an easy and effective way to reduce costs, and it makes perfect sense that Kaiser is pushing the limits here. The concerns that some technicians will lose their jobs is understandable, but I believe it is already happening in fields such as radiology which can be easily outsourced.
Improving technology and connectivity are also facilitating the shift to telemedecine beyond just video doctor visits. Labs (both third-party and within the hospital setting) can do blood work in advance or after a telemedicine visit so that the doctors will have all necessary diagnostic information at their fingertips. Though Theranos has been a pretty visible failure, I believe the day will soon come when you can do blood tests at home and send the results directly to your doctor. I don’t know if the product has hit the market yet, but there was an announced toilet that could analyze urine and send the results to your doctor – so we’re pretty close! [1]
[1] The General Practitioner Toilet. http://www.yankodesign.com/2012/05/04/the-value-of-pee/
Thank you for the post, Taylor!
You mention that “Kaiser is both the insurer and provider, from primary care to hospitals. This model incentivizes them to lower the total cost of care and hence focus on preventative health and lower cost settings.” I had no idea about this and it seems like a great model if the system truly acts towards lowering the overall cost of care. However, don’t you think that there could be a possibility of conflicting goals when certain types of treatments / procedures would yield the maximum margin for KP overall but widely differing margins for the individual verticals of insurance and provision? I would imagine a situation in which the financial goals of both these verticals not be perfectly aligned at all times and I wonder how they manage for that.
Also, given that electronic medical records are such a core part of their business, do you know if they are doing anything special to build safety from hackers, given such instances – https://krebsonsecurity.com/2016/10/europe-to-push-new-security-rules-amid-iot-mess/ and http://www.businessinsider.com/hospitals-are-becoming-targets-for-hackers-thanks-to-poor-security-2016-4
Taylor – great post. It seems like Kaiser is doing a great job at making strides to improve the painful process of seeing a doctor. I have had incredibly poor experiences lately with seeing doctors. One example is a year ago, I had the flu and used United Healthcare’s telemedicine service so that I could (hopefully) get some tamiflu. I spoke with the MD through the video camera and after 5 minutes, the MD strongly suggested I go straight to the ER because she had no way of knowing any of my vitals. I went to the ER and was told that the teledoc was just covering for herself because of the liability of giving bad advice. I felt like I was scammed! I like that Kaiser is taking the old model (real locations with nurses / nurse practitioners) so that in person analysis can be done, supplemented by the MD on the screen. This model seems much more realistic in today’s healthcare / legal environment.