Stopping a Heart Attack Before It Happens

Healthcare is shifting from reactive and intermittent health to continuous, proactive, preventative care. This transformation has the potential to save the healthcare system billions, while significantly improving patient outcomes.
Healthcare is shifting from reactive and intermittent health to continuous, proactive, preventative care. This transformation has the potential to save the healthcare system billions, while significantly improving patient outcomes.
The issue with our current way of practicing medicine is twofold: 1) patient data is limited to very occasional patient-doctor interactions, and 2) patients are assumed to be relatively uniform. This drives doctors to generalize treatments for patients; however, it is becoming ever more evident that disease manifests itself very differently in different people, requiring more targeted treatment.
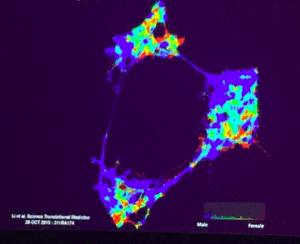
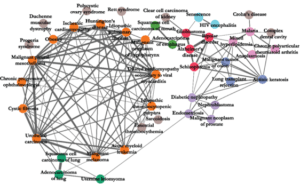
For example, scientists are discovering that diabetes may not be limited to type 1 or type 2 (see image below), or that while the standard asthma medication prescribed to millions of children and adults works well in Caucasians it can have serious adverse effects in African Americans. Similarly, a high resting heart rate may be detrimental to one patient, but perfectly normal and healthy for another. Our baselines fundamentally differ.
Segmentation analysis of type 2 diabetes patients suggests at least 3 distinct sub-types. [1]
As such, the healthcare industry as a whole needs to shift towards greater personalization*. Certain areas – oncology in particular – have already taken strides toward individually sequenced tumors and targeted therapies. Most areas, however, are lagging seriously behind.
Digital health is an attempt to change that. Major advances in home diagnostics and wearables/sensors mean that patient data can now be gathered continuously – with a doctor or AI (artificial intelligence) looking on remotely. This allows a personalized baseline to be built per patient, and thus for more targeted, well-timed and ultimately more effective treatment.
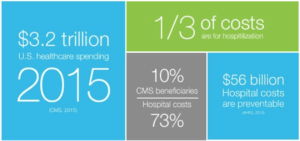
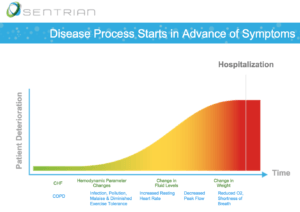
Sentrian is a startup based on machine learning and advanced sensing technology that promises to shift the paradigm of chronic care by monitoring and predicting health decline before patients require hospitalization. Hospitalization alone accounts for a third of healthcare’s $3.2 trillion spend, with $56 billion being totally preventable.
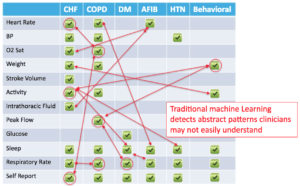
Sentrian identifies remote biosensors and wearables relevant to an individual patient’s needs. Using the data from these devices, an algorithm is run to identify early signs of health deterioration. Its accuracy stems from an understanding that chronic disease is complex and that patients often have multiple conditions interplaying. It thus takes all of these into account when assessing overall health.
[2][3]
With input from a physician team, Sentrian can tailor the algorithm to notify the physician team at a certain threshold for intervention. This reduces the rate of false alarms, but also increases the number of cases in need of treatment before they become critical.
[2]
Sentrian is currently partnering with CareMore and Scripps Translational Science Institute to test and improve their system. The 6+ month pilot with COPD patients has been able to detect “88% of hospitalizations five days in advance, with only a 3% incidence of false positives.” [4]
Sentrian is interesting because it combines AI and physician knowledge and experience into what it calls “clinician-directed machine learning”. The reason to involve the clinician is not that Sentrian innately believes in doctors’ abilities, but because it makes it easier to build and continuously improve their algorithms. If a patient were relying only on the AI, any change in algorithm would require new regulatory approval. Positioning the AI as a support to doctors, however, means that no such approval is required. As the regulatory environment adapts, this is bound to change to allow us to rely more on AI systems.
AI is already better than physicians at interpreting e.g. medical records and medical images (Enlitic), and can parse through millions of studies to find the best possible therapy for a particular patient (IBM Watson Health). Home health systems even mean that patients can self-diagnose at home (e.g. Scanadu, part of the Qualcomm Tricorder XPrize). Someday patients may even have access to their own personal health records(!), potentially stored on the blockchain for easy and secure storage and access.
As such, the digital health revolution poses an interesting conundrum for doctors. Doctors may start to become more superfluous as medical scientific experts, and instead start to play more of an emotional role in care. Pretty soon we’ll find ourselves in a world where malpractice means a doctor who hasn’t consulted an AI before diagnosing and prescribing treatment.
*Personalized medicine in this context does not necessarily mean on a per-person basis. This may be economical in life-threatening diseases such as oncology, but for most conditions “personalized” simply refers to greater patient segmentation than is currently used.
[732 words]
Sources:
- [1] Li et al, Science Translational Medicine, “Identification of type 2 diabetes subgroups through topological analysis of patient similarity”, October 2015
- [2] Sentrian
- [4] http://www.mobihealthnews.com/content/caremore-sentrians-remote-monitoring-pilot-combines-machine-learning-human-insight
- [3] Atul Butte, Singularity University; Suthram S, Dudley, …, Butte AJ. Network-based eluciadation of human disease similarities reveals common functional modules enriched for pluripotent drug targets, PLoS;
- Singularity University, Exponential Medicine Conference
- Sentrian.com



Snoop – thank you for writing this post. I find the ability of these analytical tools to take a more predictive/proactive approach to be extremely interesting and valuable for all stakeholders (consumers, insurance companies, doctors). This post reminded me of a presentation I heard earlier this semester by the founder of RapidSOS (https://www.rapidsos.com/?utm_source=Header&utm_medium=RapidSOS%20logo&utm_campaign=Website), a startup that is developing technology to predict and preempt emergencies before they occur, dynamically warn people in harm’s way, and ensure that first responders are one touch away globally. Effectively, the business is hoping to modernize the 9-1-1 infrastructure to be speedier and more predictive in order to improve health outcomes much the same some of the technologies you talk about are doing in the doctors office. I look forward to seeing these technologies developing further and improving health outcomes for more patients.
Thanks for sharing this. I’m really excited about the shift towards more preventative healthcare and think there are opportunities for all stakeholders including the general population, healthcare providers, governments, and insurance providers to benefit. I’m curious though how we’ll get over some key hurdles. Firstly, It seems like many of these predictive technologies get better with larger and more comprehensive data sets. However, I’m curious what it takes to have patients comfortable with having extensive amounts of data on them tracked and available for analysis. Data can definitely be obfuscated and evaluated at non-personal level for predictive use; however, the storage of it still leaves it at risk for data breaches. Beyond that, I’m curious how those in more difficult socio-economic classes can equally (1) provide their data (e.g., through their smartphones or fitness trackers), and (2) subsequently accessing their data and relevant insights? Lastly, I’m curious how the various data sources all come together to paint a comprehensive picture of a patient – not just medical markers but data on behaviours and consumption (e.g., fitness, nutrition, etc.). There appears to be different apps and interventions that are collecting data on specific things but I wonder how this all comes together – especially since some of the gatherers of this data might have different interests (e.g., MyFitnessPal collecting data on what you eat).