Prellis Biologics: Manufacturing Life
Prellis Biologics' holographic 3D printing of biomaterial and ethical considerations surrounding manufactured organs.
(745 Words)
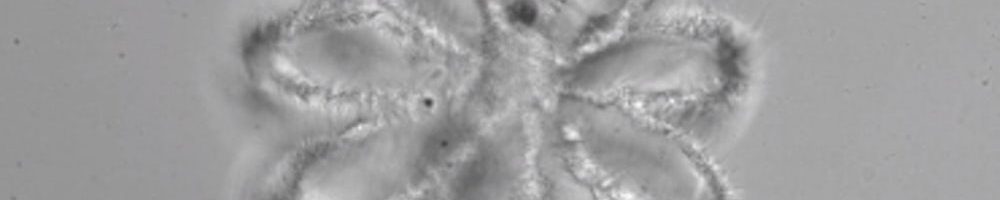
Additive manufacturing is essential to Prellis Biologics’ long-term goal of 3D printing human organs. Bioprinting of human tissue has been possible for years, however, scientists have yet to manufacture functional human organs.1 Kidneys, the toxin-filtering organs responsible for removing waste from our blood, are of particular interest to bioprinting scientists due to the chronic need for kidney donors around the world. Kidneys are provided nutrients through networks of tiny blood vessels called capillaries that supply the nephrons – the functional unit of the kidney – with blood (tissue vascularization).2 For perspective, a single kidney contains roughly one million nephrons,3 making it impossible to build viable kidney tissue with conventional 3D printing methods.
Historically, 3D printing techniques have been based on the repeated layering of extremely thin sheets of substrate. While this method is useful for a wide-range of applications and has led to innovations across sectors,4 its time-consuming nature proves incompatible with the short lifespan of human tissue outside of a nutrient-rich incubator (like a healthy human body, or a bioreactor).5 Holographic 3D printing, the technology used by Prellis, has ushered in a new frontier in bioprinting by solving this problem. Holographic 3D printing uses lasers to instantaneously and precisely (to half a micron) solidify a substrate, paving the way for the production of time-sensitive products like kidneys.6 Prellis’ management attests that they’ve overcome the biggest obstacle on the path to 3D printing organs by solving the vascularized tissue problem.7 Now, some industry experts are predicting that viable 3D printed organs could be a reality in as few as five years.8
Going forward, organizations like Prellis will have to work closely with the government to bring lab-grown organs to market in the most ethical way possible. Over time, Prellis could offer organs to patients awaiting transplant at a fraction of the emotional toll and monetary cost of waiting for one to become available from another person. In the United States, there are over 114,000 people waiting for an organ transplant, with one person added to the national transplant list every ten minutes. Waiting for a transplant can be costly – patients can expect to wait around five years for a kidney donor match.9 While waiting, patients must undergo dialysis treatments, which cost roughly $90,000 per patient per year.10 Once a donor is found – either living or deceased – testing must be done to ensure that the kidney is safe for transplant. The logistical maze hospitals go through to perform a successful transplant is navigated under direction from UNOS, the United Network for Organ Sharing. UNOS matches organs with recipients based on a number of factors, including blood type, distance (from donor to recipient), urgency, and patient compliance.11 If a company like Prellis can create an organ from a patient’s own cells, UNOS’ services might no longer be required.
Prellis should begin working with policy makers as soon as possible to create the necessary regulations required for this new phase of transplant medicine. Currently, the medical community is at a crossroads on the issue of 3D bioprinting.12 Of course, the technology will save lives, time, and money, but it also raises serious ethical questions. To start, the current process for clinical trials testing isn’t suited for specialized 3D printed organs. Regulators will need to work with the medical industry to establish a new set of benchmarks to ensure that the transplant process is safe from lab to surgery. Additionally, as the technology scales, it’s likely that only wealthy individuals will have access to it. An introduction of lab-created organs to the market of any magnitude will decrease the overall wait time of UNOS’s waiting lists. However, the situation will be such that some of the population (those who can pay) will receive an organ immediately (lab-created), and the rest must wait for a human donor, further exacerbating the inequalities in our healthcare system.
Going forward, companies like Prellis face a number of challenges: increasing competition, regulatory pressure, and concerns about scalability. Some of the most immediate questions center on Prellis’ future ability to prove the safety of their products. What is an effective framework for conducting clinical trials for 3D printed organs? How does Prellis go about determining who its first customers will be? Does the company work directly (in series) with UNOS, or parallel to UNOS in a separate process? These are only a few of the many questions that biotech companies like Prellis will have to answer as they continue to push the boundaries of medicine.
- Sean V Murphy, & Anthony Atala. (2014). 3D bioprinting of tissues and organs. Nature Biotechnology, 32(8), 773-85.
- “Your Kidneys & How They Work.” National Institute of Diabetes and Digestive and Kidney Diseases, S. Department of Health and Human Services, 1 June 2018, www.niddk.nih.gov/health-information/kidney-disease/kidneys-how-they-work.
- Britannica, The Editors of Encyclopaedia. “Nephron.” Encyclopædia Britannica, Encyclopædia Britannica, Inc., 3 July 2015, www.britannica.com/science/nephron.
- Spaeth, D. (2017). 3D Printing is Changing the Face of Multiple Industries: 3D printing has edged its way into numerous spheres, cementing its growing professional influence. ECN-Electronic Component News,61(9), 21-23.
- Jackson, Beau, et al. “Prellis Biologics Aims to 3D Print Kidney Vessels in 12 Hours or Less.” 3D Printing Industry, 21 June 2018, 3dprintingindustry.com/news/prellis-biologics-aims-to-3d-print-kidney-vessels-in-12-hours-or-less-134947/.
- “Prellis Biologics Reaches Record Speed and Resolution in Viable 3D Printed Human Tissue.”com, 21 June 2018, 3dprint.com/217267/prellis-biologics-record-speed/.
- Prellis Biologics, www.prellisbio.com/technology.
- Shieber, Jonathan. “Implantable 3D-Printed Organs Could Be Coming Sooner than You Think.” TechCrunch, TechCrunch, 25 June 2018, techcrunch.com/2018/06/25/implantable-3d-printed-organs-could-be-coming-sooner-than-you-think/.
- “Organ Procurement and Transplantation Network.” OPTN: Organ Procurement and Transplantation Network, optn.transplant.hrsa.gov/.
- “Statistics.” The Kidney Project, UCSF, pharm.ucsf.edu/kidney/need/statistics.
- “Frequently Asked Questions.” UNOS, 28 June 2018, unos.org/transplantation/faqs/.
- Haddow, J., Vermeulen, N. “So, What Is Not to Like about 3D Bioprinting?” Blog – Journal of Medical Ethics, 21 Mar. 2017, blogs.bmj.com/medical-ethics/2017/03/21/so-what-is-not-to-like-about-3d-bioprinting/.



This was super interesting, Emma! While I was reading, I thought a lot about how Prellis should move forward with clinical trials. From a manufacturing perspective, I wonder if regulators would require quality control of each printed kidney, or would they rely on the proven clinical trials of past printed kidneys as an indicator? If they require the latter, would product efficacy expire? Would Prellis need to requalify and test every year? My fear is that regulation and bureaucracy could slow this process to be equal with waiting for a human organ in its early years.
There’s a tremendous need for these transplants, so I imagine regulators would be pressured to move forward with a time-saving method to approve quality and bring this technology to market. I imagine that UNOS would be highly skeptical of printing kidneys, but I think they’re a valuable partner for logistics and distribution of organs. I’m envisioning a system similar to what exists today, but with more inputs.
Great post. This got me thinking about some of the other ethical questions that we will have to grapple with when this technology becomes reality such as when should people not receive new organs, how long should human life be, how much money is extending life worth, and many others. It will be interesting to see these topics evolve as the ability to create human organs becomes a reality.
I was not aware of the possibilities of using 3D printing to increase the supply of key human organs for those who need it most. Given how supply has always been an issue in the organ donor market I think this is an incredible advancement for our society. As I think about your questions on how should 3D printers work with UNOS, I would look at how many people on the list are statistically unlikely to get a donated organ in time. Given these people are likely in a dire situation, they are possibly going to look at opting-in to participate in clinical trials of 3D printed organs because their life may depend on it. This becomes a win win because you are increasing supply and adding hope for people who necessarily did not have it before while helping advance our society’s biotechnology capabilities.
Awesome article! What they’re doing is so interesting and possibly game changing that it makes me want to see if they need MBAs on their team. Although some might come up with ethical issues with this, I personally only see upside. Even if it takes time for the technology to be available to the masses, if it were not for the few who are ready and willing to pay for medical advances, they wouldn’t be made in the first place and then nobody would have them. Great stuff.
This is so cool – thank you for sharing this story, Emma!
It’s fascinating to think that our society has gotten to the point where there is a company trying to 3D print kidneys and technology risk (“can they build it”) is almost the least of their worries. Thanks for shedding light on the legal and regulatory issues that are some of the most complicated parts.
One question I have is to what extent people who are looking for a kidney would be willing to accept a 3D printed one. While there might be some patients who would rather wait and see if they can get a traditional kidney transplant, it’s likely others (and maybe most) would be more inclined to try this option if it means getting a kidney as soon as possible. Maybe Prellis has an opportunity to literally create a petition of potential patients that would want this as a way of sparking the regulatory and legal processes to move forward.
Agreed with Mike — this is definitely something worth working on.
Loved this article, Emma – thank you for sharing! I echo a lot of the comments above that mention trials on consumers with very high demand / who are unlikely to otherwise receive a kidney in time. I’m certainly not a medical expert, but I wonder about how insurers and doctors would view 3D printed organs given the industry’s nascent stage and the lack of knowledge on long-term risks. If something goes wrong with the organ or if there are serious side effects, who shoulders the legal responsibility? I can see hesitation from insurers to cover any of the cost and hesitation from doctors to recommend a 3D printed organ, at least until the long-term risks are clear, which would likely slow down the entire adoption process.