Mercy: Delivering better quality healthcare at a lower cost

How Mercy has leveraged its supply chain to provide better, more cost-effective healthcare
In the U.S., in order to combat unsustainable rising healthcare costs as well as push for higher quality, provider payments are shifting from fee-for-service to value-based. Essentially, since hospitals receive a fixed amount of money for a given treatment, they must adapt their cost structures if they are to be financially sustainable.
The healthcare supply chain starts from manufacturing and goes through to delivery of services to the patient. For hospitals, supply chain expenses make up around 30% of spend, representing a large cost lever [1]. In a 2015 survey, two-thirds of hospital decision makers “strongly agreed improving the effectiveness of their supply chain will reduce overall costs, increase revenue and lead to better quality of care” [2].
Mercy is a large U.S. health care system with over 2000 physicians, 44 hospitals, across 4 states [3]. Leadership at Mercy has recognized the need to innovate and digitize their supply chain and they are among the leading providers in this area [3].
Analyzing a combination of clinical and cost data enables providers to find opportunities to simultaneously reduce their expenses and enhance care quality. Mercy created a “United Analytics Platform” (UAP) which combined data from across their organization. A dashboard enables everyone to see “the total cost of care, including labor, product selection, product cost, length of stay and inventory holding costs by procedure, and compare them across the enterprise”.
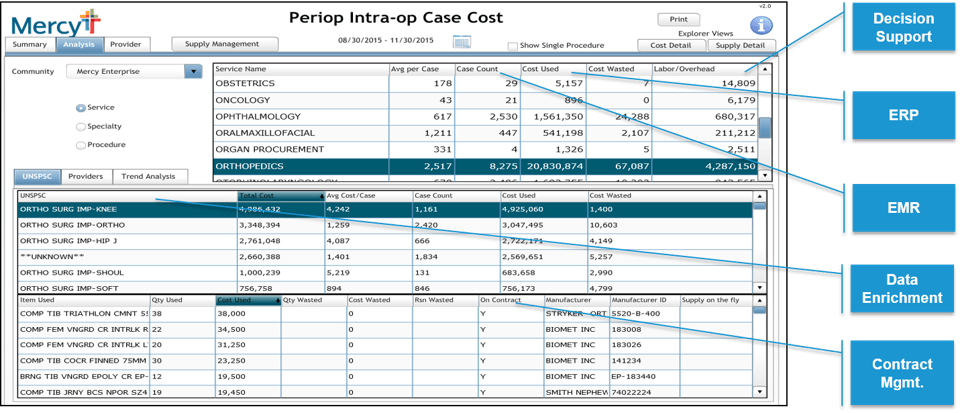
Image Source: Mercy ROi, as published in [4]
The impact of this platform has been impressive: In one case, Knee Arthroplasty, sharing trusted data with surgeons catalyzed a behavior change reducing costs per procedure from $6,500 to $5,200 over a few months [4].
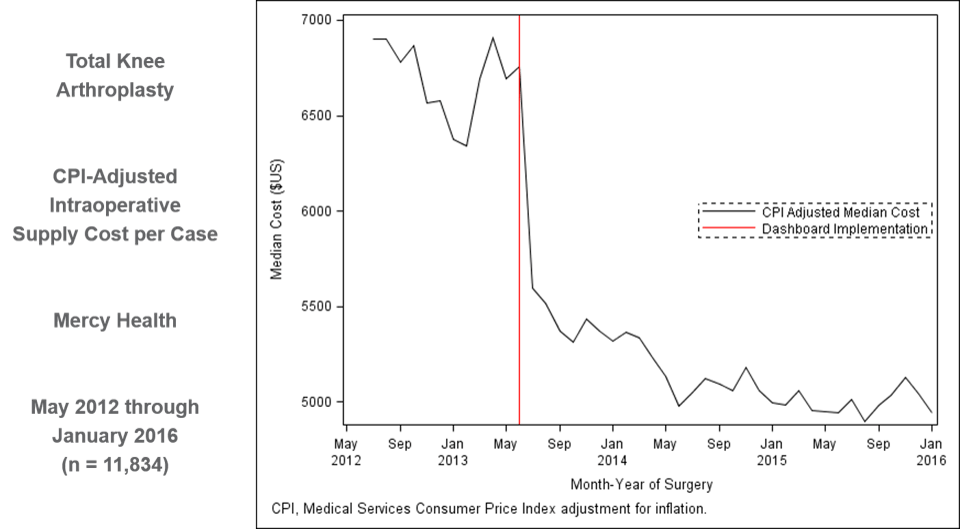
Image Source: Mercy ROi, as published in [4]
Mercy initially implemented UAP in perioperative services. They are extending this across their organization. In the short-term, Mercy plans to share this platform with its suppliers and manufacturers, in an effort to build collaborative partnerships generating further synergies [4].
Another short/medium term initiative is Mercy Virtual, the first large-scale virtual care center in the US [5]. Mercy Virtual and ROi, Mercy’s supply chain arm, are collaborating to find ways of “efficiently deliver[ing] supplies and equipment to patient homes” [6]. Incorporating telematics into the patient’s home enables supply chain responsiveness to replenish supplies or administer care, and play a bigger role in understanding underlying behavioral or environmental issues which are linked to a patient’s condition [5]. Mercy’s work can really pioneer “breakthroughs in thinking about holistic delivery from hospital to home that deliver dramatically higher satisfaction for patients with far lower costs” [7].
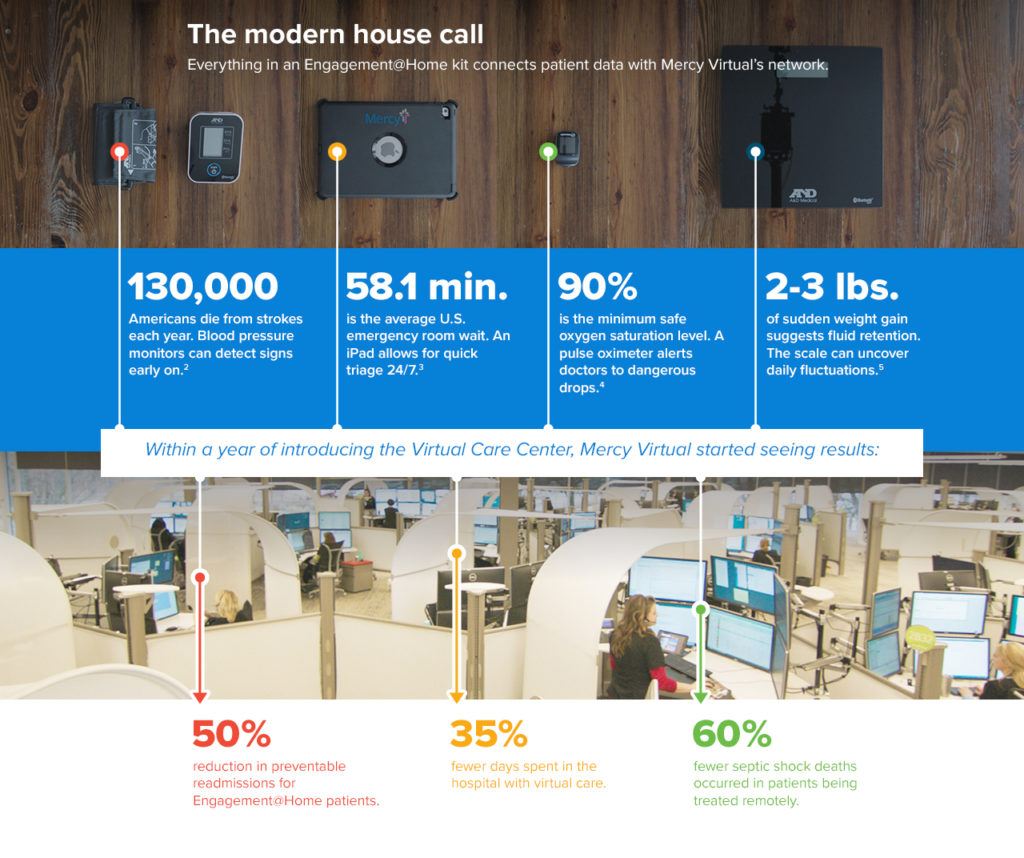
Image Source: As published in [8]
Mercy is also playing a bigger role in pushing the industry and sharing best practices. In 2010, they formed the Healthcare Transformation Group (HTG) with leading providers, such as Mayo Clinic. The first initiative of HTG is to push for adoption of GS1 standards, such as barcodes.
The group produced a video demonstrating the importance of the issue:
Video source: [9]
Long-term, Mercy along with HTG is pushing for integration of these standards, e.g. with IT solution providers of ERP and EHR [10]. This requires collaboration across healthcare providers, suppliers, and IT solution providers. In another internal initiative, Mercy is in the process of educating its own organization on the process and value of unique identification [11].
In addition to current efforts, externally, Mercy could play a role in creating interoperable EHRs across the healthcare industry. It is well-positioned to do this as among the first to adopt EHR, and a supply chain organization, ROi, which is a company itself. As patients move between hospital systems, having EHRs which translate well will enable better care delivery and potential cost savings.
Internally, it is difficult to say what else Mercy could do: Public sources of data indicate work on many fronts including predictive analytics [12][13], and further supply chain initiatives [14]. However, Mercy should be cautious of being spread too thin across several initiatives, from an economics and human capital perspective. To this end, Mercy should ensure financial astuteness in managing its cash flows as it makes large bets such as Mercy Virtual, a $54 million investment. Its operating budget is not public, however, Randal Moore, President of Mercy Virtual acknowledged the shift to telemedicine requires figuring out “how do I get from here to there without imploding and going bankrupt in between?” [15] Furthermore, Mercy should make sure it is investing heavily in creating the right organizational structure which will enable its transformations, training its workforce to be data-driven, and hiring the right talent.
Going forward, what do you think are the biggest challenges and opportunities the healthcare industry faces as it moves to the digitization of its supply chain? Is there a bigger role that insurance providers can play in this digitization, and what benefits can they absorb?
Word Count: 799
Sources
[1] Lopez, Edwin and McKevitt, Jennifer. “Study: Hospitals can save $9.9M by improving their supply chains.” SupplyChainDIVE, September 20, 2017. https://www.supplychaindive.com/news/Navigant-hospital-purchasing-study-quality-cost/505162/, accessed November 2017.
[2] Cardinal Health. “Survey Shows Hospital Decision Makers Identify Supply Chain Effectiveness Among Top Priorities.” December 14, 2015. http://cardinalhealth.mediaroom.com/2015-12-14-Survey-Shows-Hospital-Decision-Makers-Identify-Supply-Chain-Effectiveness-Among-Top-Priorities, accessed November 2017.
[3] Mercy. “Mercy Quick Facts.” https://www.mercy.net/newsroom-mercy-quick-facts, accessed November 2017.
[4] “Healthcare Supply Chainnovators 2016: Global Patient Care and Supply Chain Analytics Win the Day,” Gartner, Inc., accessed November 2017.
[5] Blake, Barry. “A visit to the future of healthcare: inside Mercy Virtual.” SCM World, A Gartner Community, March 29, 2016. http://www.scmworld.com/a-visit-to-the-future-of-healthcare-inside-mercy-virtual/, accessed November 2017.
[6] Mercy. “Forbes: Mercy Virtual and Supply Chain “Changing Health Care” for the Better.” Press release, January 30, 2017. Mercy website, https://www.mercy.net/newsroom/2017-01-30/forbes-mercy-virtual-and-supply-chain-changing-health-care-for-the-better, accessed November 2017.
[7] O’Marah, Kevin. “Supply Chain Is Changing Healthcare For The Better: An Interview With Barry Blake.” Forbes, January 26, 2017. https://www.forbes.com/sites/kevinomarah/2017/01/26/supply-chain-is-changing-healthcare-for-the-better-an-interview-with-barry-blake/2/#228f77baae7c, accessed November 2017.
[8] World Wide Technology. “Mercy Virtual Creates Anytime Healthcare.” Case study, World Wide Technology website, https://www2.wwt.com/case-study/mercy-virtual-creates-anytime-healthcare/, accessed November 2017.
[9] Intermountain Healthcare. “Data Standardization,” YouTube, published August 28, 2013. https://www.youtube.com/watch?v=g7D6pm_bLyU&feature=youtu.be, accessed November 2017.
[10] Healthcare Transformation Group. “HTG Summit 2017.” Presentation, September 27-28, 2017, HTG website. http://healthcaretransformationgroup.com/backend/wp-content/uploads/2011/10/HTG-Summit-Presentation_2017_Final-Version_Comp-v5-Final-minus-all-pictures-P1.pdf, accessed November 2017.
[11] Conway, Karen. “HTG focuses on cross-industry problem-solving.” Healthcare Purchasing News, November 15, 2016. https://www.hpnonline.com/htg-focuses-on-cross-industry-problem-solving/, accessed November 2017.
[12] Powelson, Jill. “Elevating Patient Care With Predictive Analytics.” Media Planet. http://www.futureofbusinessandtech.com/business-solutions/elevating-patient-care-with-predictive-analytics, accessed November 2017.
[13] Pecci, Alexandra Wilson. “Data Analytics Helped Mercy Slash $4.3M in Nursing Costs.” HealthLeaders Media, August 28, 2017. http://www.healthleadersmedia.com/technology/data-analytics-helped-mercy-slash-43m-nursing-costs, accessed November 2017.
[14] Bresnick, Jennifer. “Healthcare Analytics Help Mercy Uncover Cost, Quality Insights.” HealthITAnalytics, March 9, 2017. https://healthitanalytics.com/news/healthcare-analytics-help-mercy-uncover-cost-quality-insights, accessed November 2017.
[15] Wicklund, Eric. “Mercy Virtual’s President Talks Telemedicine, Value-Based Care.” mHealthIntelligence, June 16, 2017. https://mhealthintelligence.com/news/mercy-virtuals-president-talks-telemedicine-value-based-care, accessed November 2017.



Your article brings up important issues that are prevalent in healthcare today. I enjoyed learning more about Mercy’s approach and success thus far, particularly with regards to the observed change in surgeon behavior in the context of the increased cost transparency. In line with this, I think one area of focus would be at the very end of the supply chain: the physician users. As we discussed in an FRC case and also in the MKT case on Angiomax, physicians for the most part are not aware of the healthcare costs of the materials/supplies and medicines that they use for their patients. It would be interesting to see how a platform such as Mercy’s could be integrated with existing order software that is built into electronic medical record systems like Epic to augment physician ordering behavior on a hospital-wide scale. Therefore, a potential next step for Mercy could be to focus on establishing partnership agreements with these EHR companies to attempt to change ordering behavior on a large scale.
Wonderful piece; thank you for discussing both supply chain digitization within hospitals and supply/demand mismatch with patient/providers as it relates to telehealth.
With regard to the first, the UAP program’s promise is clearly cost-reducing. However the peer effect it exerts on individual physicians who will increasingly be judged transparently against their peers (see example of Surgeon Scorecard by ProPublica – https://projects.propublica.org/surgeons/) is an excellent impetus for providers to start thinking about their own performance. While individual physician’s cost reduction efforts may lag behind the times, leveraging this peer effect is the fastest way to achieve cost savings among driven, type A providers who have been educated in a system of peer comparisons.
Another system that is launching similar telehealth efforts is my own medical school’s health system – Jefferson Health System – see http://hospitals.jefferson.edu/jeffconnect.html. They used a well known telehealth platform to pilot with the lowest hanging fruit first, their own provider and workforce. By offering their own employees and constituents the ability to trial telehealth before exhausting excessive social and human capital selling the story for a patient-facing platform, leadership gained keys insights on what worked and what wouldn’t, avoiding some of the concerns you mention regarding spreading the provider systems’ resources too thinly.
To answer your final question, yes, so much stands to be gained from cooperation between payers and providers with regard to digitization and data-sharing. Unfortunately, data asymmetry is part of what makes each group effective. Providers known one thing about patients and are able to attract patients through branding and expanding, while payers know so much more about population quality metrics and what drives cost on a regional level. This situation is changing to some degree, but not fast enough. In fact, I fear that much of recent provider efforts to achieve inter-operability through their electronic medical records will only recreate a database that insurers already have. To truly unlock the value of data sharing that has stemmed from digitization, at least in the realm of health care, we need much greater cooperation.
The idea of partnering with the EHR that Damir mentioned is intriguing. I imagine that prior to bringing telemedicine online, reducing ongoing hospital costs will need to be addressed. The technology exists and could easily be added to bring some more transparency into the healthcare system. More than that it would bring standardization. Hospitals would have to decide on one single price for a good or service and not vary this by insurance type etc. This would not only help on the cost front, but would potentially galvanize a trend towards standardization more broadly which in turn would drive down complication rates etc. This technology has the potential to be disruptive in the most positive sense if used well.
Hey Sakshi – Great post! My most recent consulting role prior to HBS was working with a hospital system in the Midwest to decrease their clinical supply chain costs. That system only had 7 hospitals and they had zero communication between them as far as supply chain went! They had separate people purchasing for each of the hospitals and sometimes even different people for individual departments within the hospitals. I can’t imagine how much more money they could have saved if they had a system like Mercy’s. I know Damir mentioned partnering with EHRs but I’d be more intrigued about partnering with other hospitals. I’m wondering if they could sell or license this system to other hospitals / clinics across the country. Could be a unique way for the hospital to make money and also contribute to a lower cost of care across the country.
Sakshi, great post. I was intrigued that the concept behind Mercy Virtual incorporates just in time delivery, which is promising to reduce costs, and follows a similar trend to some acquisitions that McKesson has made. The progress they have made in reducing costs is impressive through transparency in data that almost allows the different provides to compete against each other. I believe to have the biggest possible impact, however, they will need to address interoperability of EHRs.