Memorial Sloan Kettering – a digital affair with cancer care
Physicians (and patients) are more sophisticated and connected than ever before. But how can hospitals effectively harness this wealth of health data to deliver better care?
From precision surgery, to electronic medical records, to telemedicine, few question the impact digital innovation has had on healthcare delivery. Not only are doctors (and patients) more sophisticated than ever before, they are far more connected.
However, these benefits come with their challenges, not the least of which is effective exchange and interpretation of clinical and patient-generated data. The volume of medical information doubles every 5 years [1], of which an estimated 80% of is unstructured and dispersed [2]. This may help explain why healthcare practitioners ignore 90% of the data that they themselves generate [2], and why the rate at which the latest research actually influences clinical practice in the broader oncology community is painstakingly slow.
Surfing fearlessly at the crest of this digital wave is Memorial Sloan Kettering (MSK), New York’s premier oncology treatment and research center. MSK treats over 130,000 patients across 400 unique cancer subtypes each year [3]. These are highly complex cases, requiring specialized, individualized treatment plans. Moreover, MSK sets the standard for digital innovations to deliver quality and efficient care. Here we’ll showcase two of their more exciting initiatives.
- “Watson for Oncology” – Clinical support tool
In 2011, MSK partnered with IBM to develop Watson for Oncology, a machine designed to “analyze huge volumes of (medical) information and reduce it down to critical decision points [1]” (Dr. Craig Thompson, MSK CEO).
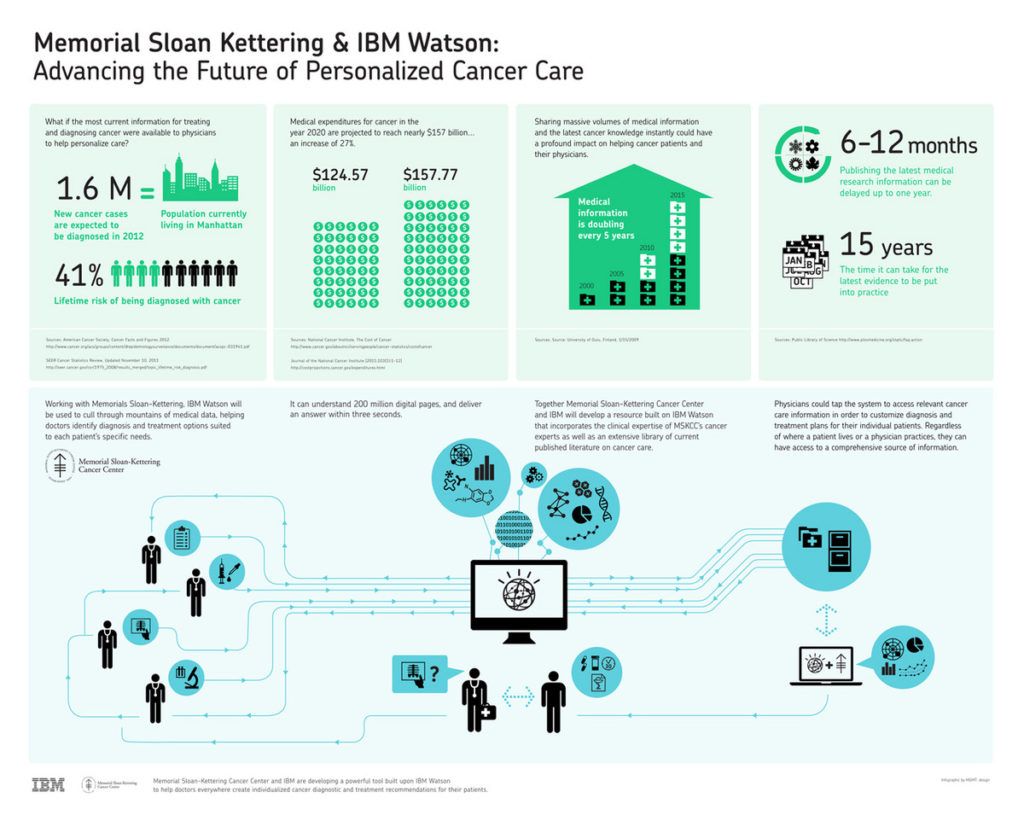
Three months after Watson defeated Jeopardy! Grand Champions Jennings and Rutter, MSK approached IBM about using Watson’s cognitive computing power to help inform clinical treatment decisions [4]. MSK had over the decades amassed thousands of patient case studies (on interventions and outcomes), the latest medical literature, and a knowledge management system designed to deliver personalized care [5]. But as MSK grows, data proliferates, and physicians are spread over a larger number of cases requiring more specialized treatment, the task of keeping up to date on the latest medical findings becomes Herculean.
Via a tablet app, an MSK oncologist would input their patient’s history, symptoms, test results, and other diagnostics, to which the program recommends a list of individualized, potential treatment plans. For each treatment option, the computer generates a degree of confidence.

For those suspicious of artificial intelligence, rest easy. Watson does not replace the physician. It lacks the empathy and critical judgment for which doctors are held responsible. MSK instead uses Watson as a means to share expert knowledge and enhance decision making, leaving the final decision on treatment to the physician.
By facilitating information flow throughout the MSK network, physicians have access at all touch points, whether in the hub inpatient facility or at one of the 21 outpatient clinics. Patient satisfaction is expected to increase as physicians now have more time to interact with their patients in lieu of tedious paperwork. And as the Watson brain learns and expands its knowledge base with further clinician input, its potential to create value for cancer patients expands beyond breast and lung cases to other cancer types like colon and bladder.
- “Versus” – Real-time location monitoring
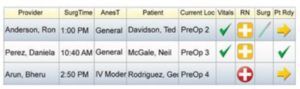
One other manifestation of the Internet of Things at MSK is the “Versus” software, a real-time location system (RTLS) currently being piloted at a few of the hospital’s outpatient clinics [6]. The primary purpose of the software is to monitor the patient’s movement through every stage of care, from admission, to procedure, to discharge.
Patients and their visitors receive a small electronic badge upon arrival that integrates location data with MSK’s OR management software, which feeds into the EMR. This greatly improves accuracy and reliability of EMR data, and frees up time for the clinician to spend with the patient.

“Glance-and-Go” electronic whiteboards throughout the facilities allow clinicians to see instantly each patient’s surgery schedule and wait time alongside OR and bed availability [7, 8]. Not only can patients move freely while remaining accessible to their clinician, clinicians are able to mitigate long wait times, prioritize care, allocate resources (like beds and staff) accordingly, and track their patients’ recovery (through metrics like post-surgical ambulation). The net benefit is an enhanced patient experience and, ultimately, superior outcomes.
***
Each of these solutions strives to improve MSK’s quality of care, streamline workflow, and optimize patient satisfaction.
The issues that arise with each align to the challenges of big data in healthcare overall. The first is data-system interoperability. That is, how do we ensure the proliferation of data is actually exchanged, interpreted, and actioned upon. By extension, does the cost of harnessing this data justify its collection? The other primary risk is one of privacy. Has the race to innovate ignored patient consent? After all, isn’t having one’s movement in a hospital tracked constantly plain creepy?
Whatever the case, as healthcare becomes increasingly democratized, the patient plays a central role in digital-enabled care innovation.
(Word Count: 792)
[1] “IBM Watson helps fight cancer with evidence-based diagnosis and treatment suggestions”. Anon. http://www-935.ibm.com/services/multimedia/MSK_Case_Study_IMC14794.pdf . Jan 2013. Web. Accessed Nov 16.
[2] “Smart use of big data: the key to the future”. Anon. https://www.healthcare.siemens.com/magazine/mso-big-data-and-healthcare-2.html . Aug 12, 2015. Web. Accessed Nov 16.
[3] “Fact and figures”. Anon. https://www.mskcc.org/pressroom/facts-figures . nd. Web. Accessed Nov 16
[4] “Learning machines: Watson could bring cancer expertise to the masses”. David Kerr. http://www.huffingtonpost.com/david-kerr/learning-machines-watson-_b_1388429.html . Mar 29 2012. Web. Accessed Nov 16
[5] “What’s your strategy for managing knowledge?”. Morten T. Hansen, Nitin Nohria, Thomas Tierney. https://hbr.org/1999/03/whats-your-strategy-for-managing-knowledge . March 1999. Web. Accessed Nov 16
[6] “Versus Advantages™ Improves Patient Experience at Memorial Sloan Kettering Cancer Clinics”. Versus. http://www.versustech.com/rtls-news/press-releases/versus-advantages-improves-patient-experience-at-memorial-sloan-kettering-cancer-clinics/ . March 11, 2015. Web. Accessed Nov 16.
[7] “Memorial Sloan Kettering’s Josie Robertson Surgery Center Innovates New Uses for RTLS”. Anon. http://www.prweb.com/releases/hospital/patientflow/prweb13256104.htm . March 10, 2016. Web. Accessed Nov 2016
[8] “Memorial Sloan Kettering facility uses RTLS to monitor patient recovery”. Claire Swedberg. http://www.rfidjournal.com/articles/view?14250/ . March 29, 2016. Web. Accessed Nov 2016
Exhibit 1: https://www.mskcc.org/blog/msk-trains-ibm-watson-help-doctors-make-better-treatment-choices
Exhibit 2: http://fortune.com/ibm-watson-health-business-strategy/
Exhibit 3: https://www.mskcc.org/blog/five-innovations-helping-msk-transform-outpatient-surgery-2016



Ben, thanks so much for sharing. Memorial Sloan Kettering is a fabulous institution, and they have taken numerous strides (many of which you’ve noted) towards leveraging data and technology to advance oncological care and business operations.
Regarding Watson, I would be quite curious to hear about any outcomes-based studies that have been conducted. For instance, do patients get matched to their rare cancers more rapidly thus accelerating time to treatment and decreasing intermediary appointments? Do patients get spared unhelpful clinical trials because of their particular characteristics, thus saving them from unwanted side effects without the hope of useful treatment? Basically, what exactly has resulted from leveraging Watson aside from saving lit-review time? Moreover, I wonder how they and IBM are monetizing this opportunity.
Ben, thanks for providing insights on technologies healthcare is using to improve its efficiency! Partnering with IBM Watson was an innovative way for MSK to leverage all the data they generate. It’s a shame not to utilize the massive amounts of patient data the hospital has generated over the years. In a time where healthcare costs are continuously increasing and doctors flooded with a minimum number of patients per hour they have to see on top of massive amounts of paper work, anything that increases “utilization” of doctors time spent with patients is welcomed. With regards to the “Verus” system, while it does feel a bit creepy to track this amount of patient data, that is unfortunately a downside of big data. As consumers, our spending habits, traffic patterns, and nearly every app we use collects and stores data about us. As long as the information is kept private and utilized properly, I think the system has potential to increase flows within hospitals.
There is an interesting opportunity and threat that results from partnerships between companies like IBM and healthcare organizations like MSK. On the one hand, patients able to receive care at MSK receive the most advanced cancer care available. This is of course a positive outcome. On the other hand, patients who are not able to receive care at MSK are relegated to treatment centers with less advanced diagnosis and treatment protocols. This triggers the potential for inequality in care, and threatens the democratization of healthcare that healthcare IOT promises to promote. IBM and MSK should be measured on how quickly they can help disseminate the lessons and best practices they have developed to other centers, so that more patients can benefit. While researching my post I came across a similar strategic alliance between Radboud University Medical Center and Philips (See Shipilov, A. A Better Way to Manage Corporate Alliances. Harv. Bus. Rev. (2014).) While providing substantial benefits to patients at the pilot center, such alliances can drive the most benefit if they are complementary and not exclusive. It would be a shame if IBM could not partner with other medical centers because they have already entered into another partnership with a similar digital partner. As healthcare IOT matures, there is an opportunity for business model innovation. Structuring win-win alliances that are complementary, and help to accelerate the positive impact of healthcare IOT would accelerate the overall uptake of healthcare IOT and maximize value for patients, healthcare providers and payers.
Thank you for sharing this fantastic article. Most of the innovations you point out seem to be from structured data collected as well as unstructured data from studies. I wonder how far they’ve come using unstructured data from the doctors’ and nurses’ notes. Each patient carries copious amounts of information that is usually ignored, primarily because of the volume. There may be leading indicators we’ve not discovered because humans simply miss them or don’t connect them to future complications. I think there is a lot of value to be gained from looking at data that humans can not analyze at scale.