From the Hospital to the Home: BIDMC’s app efforts

A leading Boston hospital seeks to improve patient care by monitoring patients via mobile apps
Overview
Beth Israel Deaconess Medical Center (BIDMC) is a teaching hospital of Harvard Medical School located in Boston on the forefront of medical research and innovation[1]. The hospital has nearly 700 licensed beds and sees nearly 50,000 inpatients per year. It is one of the top three recipients of funding from the National Institutes of Health, a key indicator of its commitment to innovation.
Hospitals and BIDMC in particular have been trying to capitalize on increased digitization to find ways to improve patient care. BIDMC has already implemented an electronic medical record (EMR) to catalog information about patients in a standard way during each visit. Now they are looking to improve care while patients are not in the hospital by collecting information in between visits[3].
Recent Digitization Efforts to Improve Patient Care
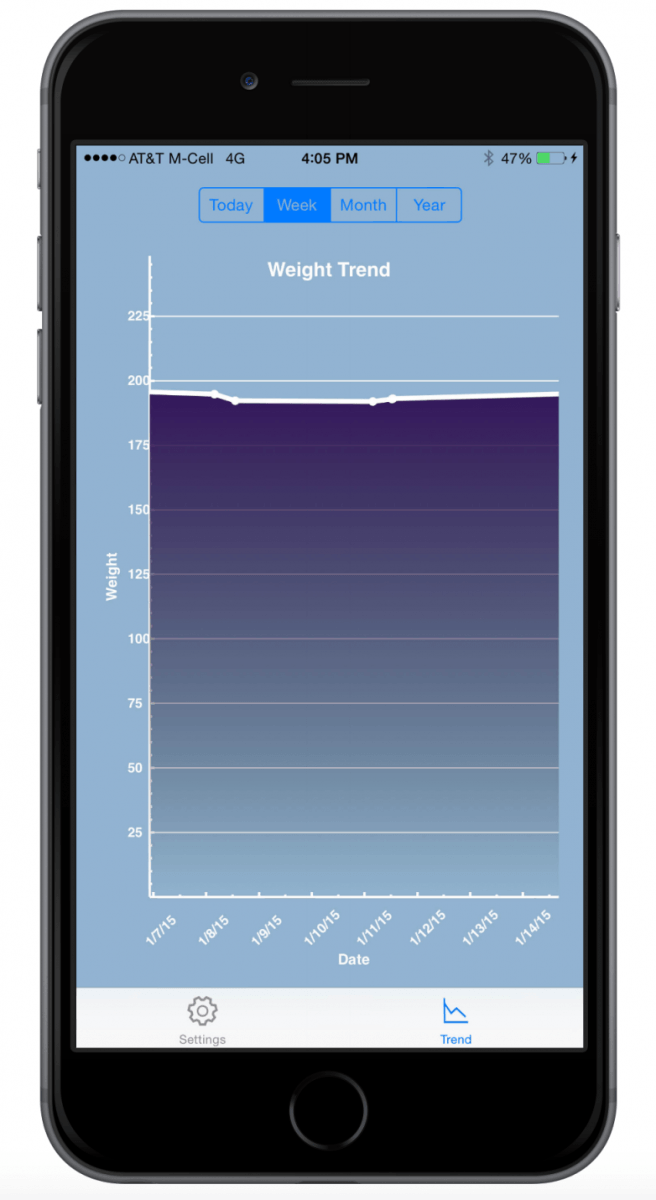
In early 2016, BIDMC announced a pilot using Apple’s HealthKit and their own app, BIDMC@Home, to connect patient data collected at home directly to the patient’s EMR. The pilot started for patients with congestive heart failure and hypertension. Scales will measure changes in weight, which could signal potentially dangerous fluid imbalances. Blood pressure cuffs in the patient’s home can be used to monitor blood pressure. Both devices will connect to the app deliver data to the EMR and the patient’s care team. The hope is that additional data collected between visits will give doctors a more holistic view of a patient’s health and will alert the doctor to any life threatening changes. The app will help doctors identify potential issues before they become too serious, which has the potential to reduce hospital readmission rates.
Recently, BIDMC announced it would leverage Apple’s CareKit software framework to collect subjective data points along with the objective measurements from patients. The app will now allow patients to input how they are feeling each day or how much pain they are in[4]. Once set up, the app will connect directly with a patient’s EMR, eliminating the need for a patient to recall at their next visit how they felt any particular day. Thus, the app will allow doctors to monitor patients’ overall wellbeing, without requiring a follow-up visit.
Other Potential Opportunities
BIDMC is piloting its app with patients suffering from congestive heart failure and hypertension3. Going forward, BIDMC can expand its digitization efforts to help patients managing other chronic conditions like diabetes. In the future, the app may be able to do more complex monitoring of patients after being discharged from the hospital. BIDMC can continue to build out more features to monitor its patients through additional connected devices like Fitbits. Finally, BIDMC can expand the functionality of its apps by creating more opportunities for two-way communication between the patient and the care team.
Potential Concerns
Access
BIDMC’s program relies on patients using their own iPhones and internet connections to transmit the data to their healthcare provider. As BIDMC scales the program, they should consider how to provide it to those who may not have a smart phone or consistent access to internet5.
Adherence
The value of detailed information on a patient between visits is high. However, the program relies on patients setting up the app and continually weighing themselves, measuring their blood pressure, and inputting how they are feeling. People may not be used to measuring themselves which may lead to issues with adherence. However, the app may be able to send reminders to encourage compliance or notify doctors or nurses when a patient stops collecting data so that they can try to intervene.
Volume of Data
With daily collections of multiple metrics, the volume of data available for each patient will increase significantly. BIDMC’s EMR will need to be ready to handle the influx of data and doctors need to be able to make sense of it[5]. BIDMC will need to develop algorithms or consolidated reports to provide doctors with more actionable data so as not to overwhelm them with the quantity of information available.
Data Security
Given the application is transmitting highly personal data and subject to HIPAA, there is a great risk to the hospital should the data be compromised5. Security measures must be in place so that patients are willing to participate in the program and believe that their sensitive data is protected.
Conclusion
BIDMC should continue to expand its digital apps to improve patient care. The potential care improvements from increased information far outweigh the potential issues with implementation. Once the pilot programs prove the model successful, BIDMC can help other hospitals roll out similar programs to improve care for their patient populations.
(758 words)
[1] http://www.bidmc.org/About-BIDMC/Stats-and-Facts.aspx
[2] https://www.healthit.gov/providers-professionals/how-attain-meaningful-use
[3] http://www.mobihealthnews.com/content/beth-israel-gears-launch-healthkit-enabled-remote-patient-monitoring-program
[4] https://medtechboston.medstro.com/blog/2016/04/06/with-help-from-apple-bidmc-ramps-up-patient-engagement-efforts/
[5] https://www.statnews.com/2016/01/19/iphone-apps-track-health/



Thanks for sharing. It is very interesting to see how hospitals are incorporating new technology from our smart phones. A key question that I have is, what (if anything) will the hospitals do with this data? I am a little skeptical that doctors, who are already very busy, will have the time to review data being transmitted from a patient’s phone to the EMR. During my time with CVS (where I helped implement technological improvements, connecting CVS to the doctor’s EMR), we found that it is doctor’s are driven by urgency and that doctors most often will not check the EMR for a patient that they are not seeing (especially one that has an appointment a few weeks out!).
Additionally, as I often find with my Fitbit, it is very easy to fudge health data (e.g. if I know my blood pressure was going to my doctor, I would only take it when I knew I was very relaxed). Overall, it will be very interesting to see how the medical profession moves with the times and finds ways to incorporate technology and keep the patient connection at home.