Digitizing Evidence: Improved health equity and optimized clinical outcomes

Digitizing Evidence: Improved health equity and optimized clinical outcomes
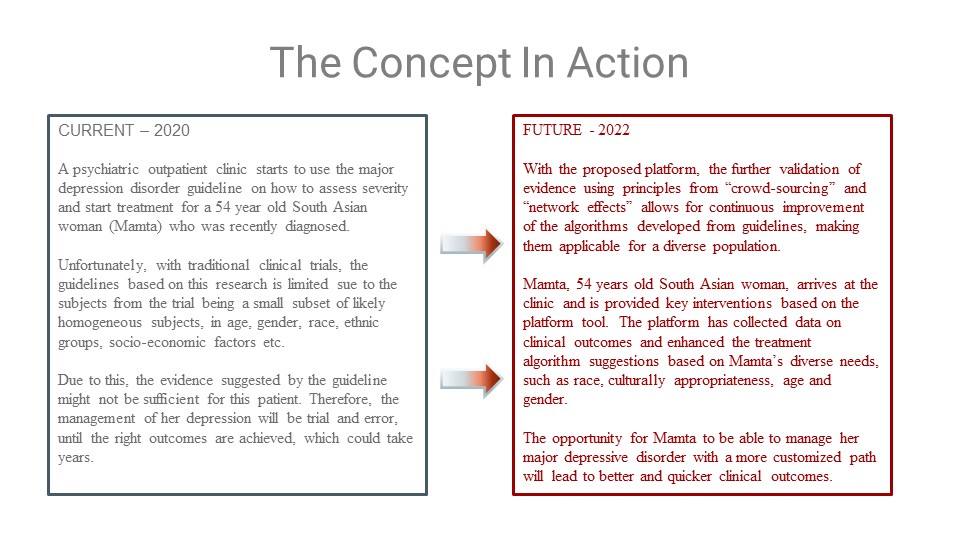
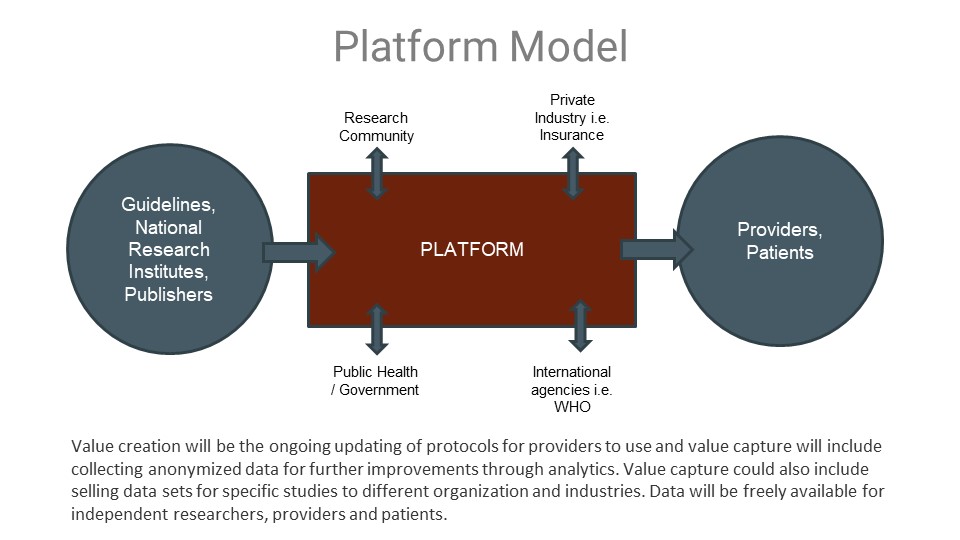
A proposed platform utilizing data science principles to further validate outcomes from clinical research and make it accessible for a diverse population.
I am a strategic healthcare executive with deep operational experience and a track record of leading clinical transformation and award-winning clinical care innovation. Colleagues know me as a results-driven professional with over 15 years of experience leading healthcare strategy, implementation, evaluation and sustainability. I am passionate about optimizing patient care through physician engagement, service integration, technology and strategic partnerships.
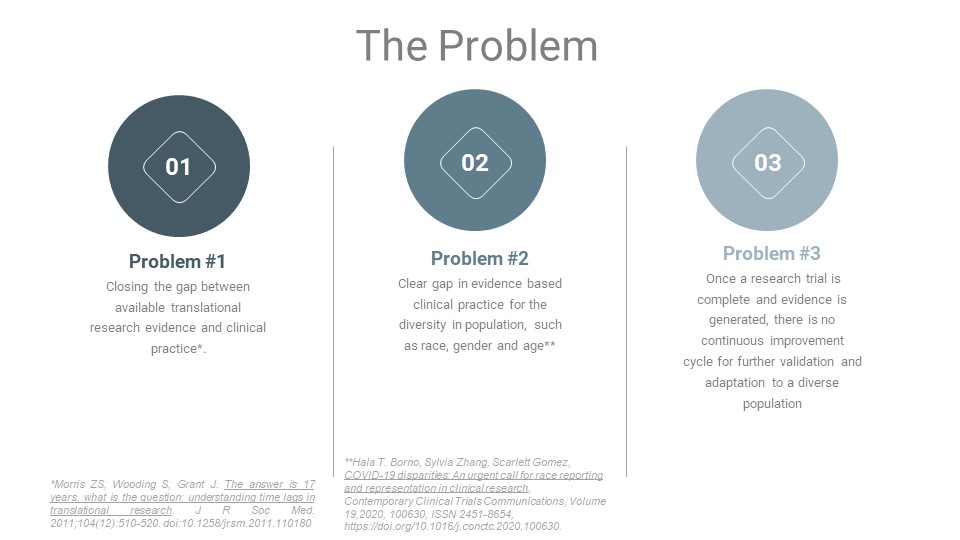
The Problem
There is a clear gap in care from a health equity perspective and access to timely quality clinical care for specific disorders. A number of applications are available to guide a provider through the clinical care based on a guideline, however, this can be enhanced exponentially by introducing a platform model which will lead to better clinical outcomes for ALL.

We are at the right moment in time, with the right technology, expertise and a burning platform to establish a goal of setting up such a platform and ensure the disruption of the traditional clinical research model, which leads to delays in access to quality care and does not address health equity.
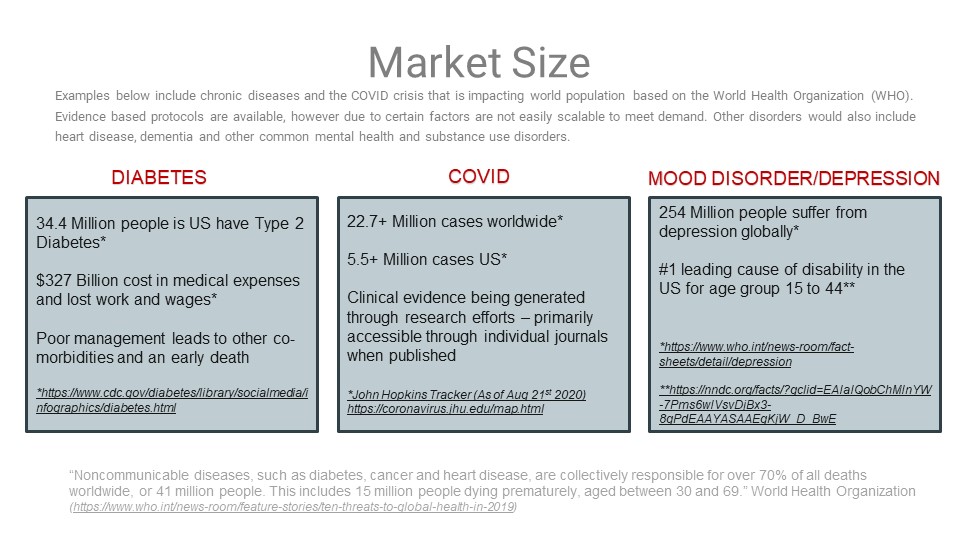
The above example only include three major health issues facing us globally. The market for this type of platform is much larger when looking at other chronic diseases, such heart disease, cancer care, mental health and substance disorders, dementia etc. On a regular basis more evidence through research is generated, however it is inaccessible to a common provider, especially in the primary care or community setting.
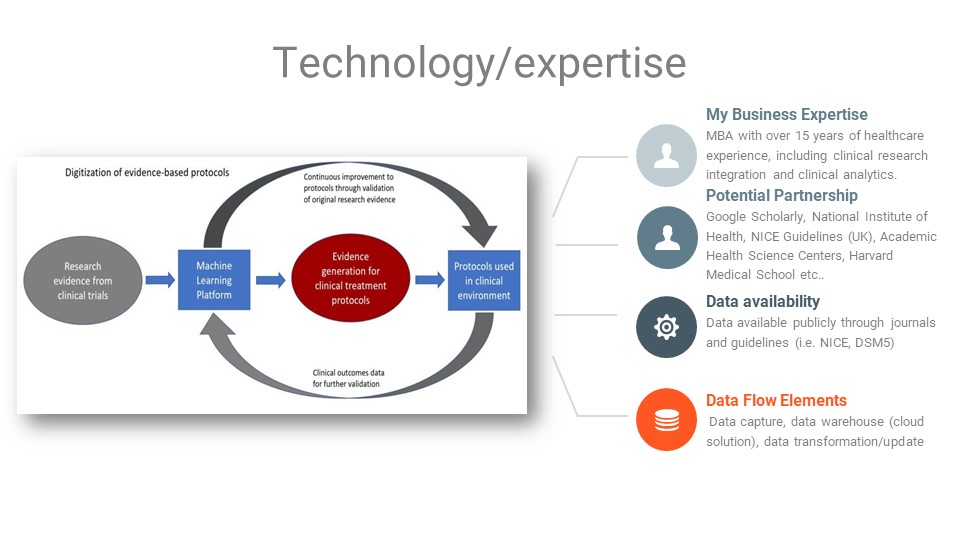 This is the initial concept of a platform that would further validate evidence based practice within a clinical environment and make it relevant for a diverse population.
This is the initial concept of a platform that would further validate evidence based practice within a clinical environment and make it relevant for a diverse population.



References (in order of content:
Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510-520. doi:10.1258/jrsm.2011.110180
Hala T. Borno, Sylvia Zhang, Scarlett Gomez, COVID-19 disparities: An urgent call for race reporting and representation in clinical research, Contemporary Clinical Trials Communications, Volume 19,2020, 100630, ISSN 2451-8654, https://doi.org/10.1016/j.conctc.2020.100630.
https://www.cdc.gov/diabetes/library/socialmedia/infographics/diabetes.html
John Hopkins Tracker (As of Aug 21st 2020) https://coronavirus.jhu.edu/map.html
https://www.who.int/news-room/fact-sheets/detail/depression
https://nndc.org/facts/?gclid=EAIaIQobChMInYW-7Pms6wIVsvDjBx3-8gPdEAAYASAAEgKjW_D_BwE
https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019


This is at its heart a philosphical question- intitution honed over years of clinical experience (aka diagonsis) versus wisdom of the crowd problem. However most medical professionals follow up on thier diagnosis through diagonostic testing and validation.
Thank you for you comment Suresh. I have developed clinical protocols based on evidence and they are not supposed to replace clinical judgment, instead it is to provide additional information to make an informed decision. Much of medicine is guideline based (developed by physicians and scientists), include decision making tools within disease specific pathways such as Cancer. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037940/
Evidence medicine has existed for a while, my proposal is to enhance it and make it more equitable and accessible through a platform.
The American Health care system is very expensive, even compared with similar countries. How this solution can help to reduce the systemic costs?
Thank you for your comment Liliam, the whole concept behind this innovation is to be more preventative and have early access to appropriate evidence based intervention at the beginning of a chronic disease trajectory. Healthcare costs are most expensive when chronic diseases are poorly managed and lead to multi-morbidities (i.e. poorly managed diabetes could lead to blindness, amputation, kidney failure), requiring more hospitalization in general, and other service utilization down the road. Coming from a Canadian healthcare system, an inpatient hospital stay for one night costs around $3000, which is likely similar in the American system. With a platform that provides better access to evidence for disease management to primary care, along with a continuous improvement cycle of updates based on clinical outcomes from a diverse population using these guidelines, one key outcome will be more appropriate healthcare utilization and cost savings.
Saima, very interesting concept. This could be hugely applicable for the pediatric demographic as well since those trials either rarely happen or are very difficult.
Thank you for your comment Stacy. I agree, especially as we are seeing more prevalence of certain disease and disorders in pediatric population – such as depression and diabetes. And there is a lack of direction of evidence on how to guide treatment.